Episode 184: Pregnancy Planning for Patients Taking Psychiatric Medications or with a Mental Health History
By listening to this episode, you can earn 1.25 Psychiatry CME Credits.
Other Places to listen: iTunes, Spotify
Article Authors: Cara Jacobson, Kristin Lasseter, MD, David Puder, MD
There are no conflicts of interest for this episode.
In this episode, Dr. David Puder, Dr. Kristin Lasseter, and medical student Cara Jacobson discuss treatment of psychiatric illness in the peripartum period.
Dr. Kristin Yeung Lasseter is a renowned reproductive psychiatrist who has dedicated her career to the intersection of mental health and reproductive medicine.
As the founder of Reproductive Psychiatry and Counseling, Dr. Lasseter has been instrumental in expanding access to reproductive psychiatry services in Texas but also worldwide through her teaching and online presence. Through her steadfast devotion to comprehending the singular hurdles faced by individuals as they navigate the reproductive journey, she has garnered immense respect within the field.
Dr. Kristin Yeung Lasseter's profound contributions to advancing women's mental health in Central Texas have been recognized through the prestigious Association of Women Psychiatrists Symonds Fellowship in 2018. Through her expertise, compassion, and advocacy, she is transforming lives and dismantling the stigma associated with perinatal mental health.
Of note, this episode, and the article below is for information purposes only and we recommend talking with a specialist doctor when considering what is the risk and benefits of particular medications in an individual's specific situation.
Risks Of Untreated Peripartum Mental Illness
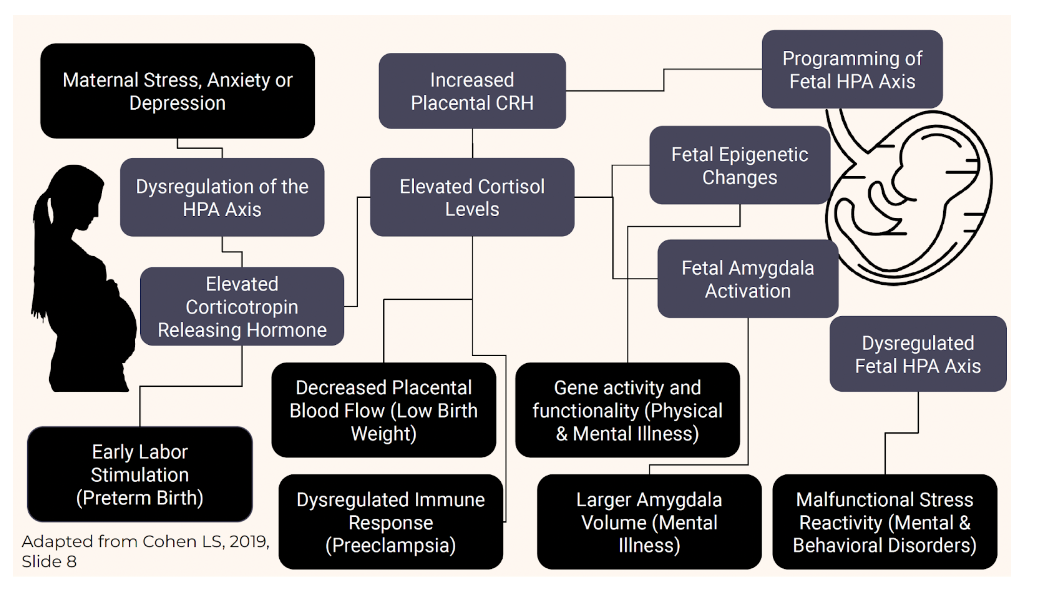
Untreated and active mental illness adversely affects both mother and fetus; therefore, it is vital to appropriately assess and treat perinatal mental illness for better outcomes for both.
There is a myth that pregnancy is protective against psychiatric illness, but mental health conditions, including suicide and overdose/poisoning related to substance use disorder, account for a larger share of all US pregnancy-related deaths (23%) than any other cause (Centers for Disease Control [CDC], 2022).
Untreated depression in pregnancy is one of the strongest risk factors for postpartum depression, which can have devastating consequences like suicide and infanticide (Payne, 2021).
More pregnant women die from suicide than hemorrhage or preeclampsia (Viswanathan et al., 2021).
Perinatal mental illness is associated with many additional adverse outcomes, including preterm delivery, pre-eclampsia, gestational diabetes, small-for-gestational-age (SGA), fetal distress, neonatal hypoglycemia, adverse neurodevelopmental outcomes, impaired maternal-infant bonding, disordered attachment, infantile colic, and increased use of harsh discipline (Betcher & Wisner, 2020; Payne, 2021).
Psychiatric illness is also associated with high-risk maternal behaviors during pregnancy, like indiscriminate sex and exposure to sexually transmitted infections, substance use, less prenatal care, and poor nutrition (Betcher & Wisner, 2020).
Systematic review and meta-analysis of 191 eligible studies with a combined sample of 195,751 unique mother-child dyads found that offspring of mothers with perinatal depression or anxiety had impaired social-emotional, cognitive, language, motor, and adaptive behavior development, extending beyond infancy and into adolescence (Rogers et al., 2020).
Children exposed to peripartum depression have higher cortisol levels, a finding that lasts into adolescence; antenatal depression treatment may result in more normal cortisol levels in infants (Payne, 2021).
See also:
Dr. Edward Tronick’s Still Face Experiment
Psychiatry and Psychotherapy Podcast episode on disorganized attachment
Psychiatric Medication In Pregnancy
Unfortunately, overall quality of evidence on the risks of psychiatric medications in pregnancy is low and confounded by the effects of the underlying conditions. This is illustrated by a 2021 systematic review of psychopharmacotherapy in pregnant, postpartum, or reproductive‐age women in which 95% of the included studies reporting on adverse effects were observational and could not fully account for confounding variables (Viswanathan et al., 2021).
However, it is clear that there are significant harms associated with untreated perinatal mental illness and we know that discontinuing psychiatric medication in pregnancy is associated with relapse of mental illness; in particular, there is a 60-70% risk of relapse in pregnant women with a history of major depressive disorder who discontinue antidepressants and an 80-100% risk of recurrence in women with bipolar disorder not taking medication compared to 29-37% chance in women continuing treatment with mood stabilizers while pregnant (Payne, 2021). Thus, it is important to appropriately screen for and treat perinatal psychiatric illness.
Deciding whether or not to start or continue perinatal psychiatric medications requires ‘risk-risk’ analysis. In general, both patients and clinicians tend to overestimate medication risks in the peripartum period but underestimate the risks associated with untreated psychiatric illness (Horan et al., 2022). Certainly, all patients do not require medication, and psychotherapy, for example, is an effective treatment in appropriately selected patients, but for those with features like moderate-severe symptoms, suicidality, or functional impairment (e.g., inability to care for self or baby), medication is likely indicated.
According to Payne (2021):
When possible, it is ideal to make changes 6-12 months prior to attempting pregnancy to ensure mood stability.
Minimize the number of medications if possible, considering the patient’s history and potential negative effects of psychiatric illness on the child.
Most psychiatric medications can be continued in pregnancy.
Bottom line: if the patient is psychiatrically ill, treat the illness.
When caring for patients with unplanned pregnancy (Payne, 2021):
See the patient as soon as possible.
Do not stop all psychiatric medications immediately.
Consider stopping teratogenic medications.
If discontinuing a medication, taper when possible.
If switching medications, remember baby will be exposed to at least 2 drugs, in addition to the risk of potential relapse.
Psychiatric Medications In Lactation
Although the benefits of breastfeeding on both maternal health and child development in general have been clearly established, there is little definitive evidence on the safety of most medications in nursing mothers, impacts on infant development, or the effects on lactation itself (Jordan et al., 2022). Research on pharmacotherapy and lactation is limited due to various factors, including lack of standardization in population databases, bidirectional effects of breastfeeding and medication use, prenatal medication exposure, and the direct impacts of breastfeeding (or not) on infant health and development, which “may obscure the true relationship between medicine exposure during pregnancy and developmental outcomes” (Jordan et al., 2022). The beneficial effects of breastfeeding may, in fact, offset some of the potential harms of medication exposure through pregnancy or lactation.
For infants already exposed in utero, Payne (2021) proposes that it may be unnecessary to switch while breastfeeding unless:
The patient experiences relapse or the current regimen is not working
Risk of severe side effects with continued exposure (e.g., clozapine)
Infant experiences medical complications or side effects from the medication during breastfeeding
Sedation is the most common side effect.
Monitor for sleepiness or poor feeding, especially when breastfeeding after a maternal medication dose.
If applicable, monitor infant blood levels.
While uncommon, antipsychotics can cause stiffness, cogwheeling, and EPS in the baby.
Psychotropic medications pass into breast milk to varying degrees. For example, sertraline is secreted in low amounts, but lithium secretion is relatively high:
For exclusively breastfeeding mothers taking sertraline, the estimated infant dose is 0.5% of the maternal weight-adjusted dose (Drugs and Lactation Database (LactMed®) [LactMed], 2022c).
A case series of 11 breastfeeding mothers found that the infant dose of lithium ranged from 0 to 30% of the maternal weight-adjusted dose, with an average of 12.2% (LactMed, 2022m).
Further details are discussed later in this article, but as a broad overview:
Most antidepressants can be used in lactation, and generally, breastfeeding mothers needing antidepressant medication should take one that has previously been effective for them (Anderson, 2021).
For breastfeeding patients requiring mood stabilizers, lamotrigine can be used (LactMed, 2022e). Valproic acid also appears to be safe in lactation (LactMed, 2022k), but other agents are preferred in women that can become pregnant given its teratogenicity. Lithium can be used in lactation, as well, particularly in healthy, full-term infants (especially those over 2 months old), although this may require close monitoring of infant behavior and/or blood levels (LactMed, 2022m).
Some anxiolytics can decrease breastmilk supply or cause sedation in breastfed infants, requiring close monitoring (LactMed 2021a, 2021b, 2022g, 2023b, 2023c).
There is less research on antipsychotics, but second generation antipsychotics seem to be relatively safe in lactation, with the exception of clozapine, which has been shown to cause adverse effects in breastfed infants (Uguz, 2016). Some antipsychotics may also increase or decrease breastmilk supply due to dopamine blockade (LactMed, 2022f, 2022i, 2022j, 2022l, 2023e).
Stimulant medications for ADHD, in particular methylphenidate, can be used in nursing mothers who require treatment (LactMed, 2023d).
Methadone and buprenorphine can be used in lactation for opioid use disorder (Nagpal et al., 2020).
The American Academy of Pediatrics (AAP) recommends against parents sharing a sleeping surface with infants (bed sharing) due to the risks of sudden infant death syndrome (SIDS), strangulation, suffocation, and entrapment and notes that the baseline risk increases by more than 10 times when someone in the bed has impaired alertness or is less able to arouse due to fatigue, substance use, or sedating medications, including certain antidepressants and other psychiatric medications (Moon et al., 2022). Bed sharing is sometimes referred to as co-sleeping, although this term is imprecise and can also refer to room sharing, where parents sleep in the same room as the infant but on separate sleep surfaces, which is recommended by the AAP and may decrease the risk of SIDS by up to 50%. Of note, they also report that breastfeeding is associated with decreased risk of SIDS.
Further resource: LactMed®
Drugs and Lactation Database (LactMed®) is a fully-referenced database that provides information about levels of drugs and other substances in breastmilk and infant blood, possible adverse effects on nursing infants, and appropriate therapeutic alternatives.
Antidepressants
Deligiannidis & Freeman (2014) report that women are about twice as likely as men to have major depressive disorder (MDD), and approximately 1 in 5 women experience perinatal depression. When left untreated, antepartum depression increases the risk of obstetrical and neonatal complications, and postnatal depression has been found to significantly negatively impact child development (Deligiannidis & Freeman, 2014).
Numerous observational studies have examined the neurodevelopmental impacts of prenatal antidepressant exposure, and several have suggested adverse effects on children’s language, cognition, and academic performance. However, these deficits are generally mitigated or eliminated when controlling for maternal depression and other confounding factors (Andrade, 2022).
A recent study of standardized exam performance in children aged 9-15 found no change in language scores and a small but significant decrease in math scores (~2 points out of 100) associated with gestational exposure to antidepressants (Andrade, 2022). These findings persisted but were attenuated when accounting for various confounders. It is likely that the remaining deficits after adjustment in this and other studies result from “residual confounding from unmeasured behavioral and internal environment variables associated with untreated maternal depression” (Andrade, 2022). Overall, it appears that prenatal antidepressant exposure may in fact be only a marker of maternal depression and not a direct cause of neurodevelopmental deficits, which seem to result primarily from the consequences of underlying mental illness, rather than medication effects.
While the existing literature does not support withholding antidepressants in perinatal depression, it remains important to use shared decision-making in conversations about medication use (Andrade, 2022).
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs have been studied the most and are the most commonly used antidepressants in pregnancy or lactation, including: fluoxetine (Prozac), citalopram (Celexa), escitalopram (Lexapro), and sertraline (Zoloft).
Neonatal Adaptation Syndrome
All SSRIs carry increased risk of neonatal adaptation syndrome (NAS), a self-limited, frequently mild condition presenting similarly to withdrawal, typically presenting with symptoms like irritability, jitteriness, respiratory distress, seizures, and hypoglycemia (Muzik & Hamilton, 2016).
Several studies have linked exposure to SSRIs in late pregnancy with transient neonatal distress syndromes thought to be caused by withdrawal from antidepressants and possibly affecting ~25% of babies with prenatal SSRI exposure close to the time of delivery (Massachusetts General Hospital [MGH] Center for Women’s Mental Health, 2022).
Symptoms include: tremors, restlessness, increased muscle tone and increased crying, but these syndromes appear to be benign and resolve quickly–within 1-4 days–without medical intervention (MGH Center for Women’s Mental Health, 2022).
Limitations include that most studies did not blind the mother’s treatment status, possibly leading to more precautionary admissions to special care nursery in infants with known medication exposure but no serious clinical manifestations, and maternal mood was not assessed, resulting in confounding, as untreated antenatal depression and anxiety are known to contribute to poor neonatal outcomes, including premature delivery and low birth weight (MGH Center for Women’s Mental Health, 2022).
Persistent Pulmonary Hypertension
Persistent pulmonary hypertension (PPH) is a serious condition affecting newborns in which high blood pressure in the pulmonary arteries leads to inadequate oxygenation of the blood. There are reports of increased PPH with SSRI exposure, but results were not clinically significant, and the risk appears to be lower than originally thought (Muzik & Hamilton, 2016).
Some studies have also found an association between SSRI use after 20 weeks gestation and increased risk of persistent pulmonary hypertension of the newborn (PPHN), but the estimated risk is small, affecting less than 1% of infants exposed to SSRIs, and subsequent studies have not found a link between antenatal antidepressant use and PPHN (MGH Center for Women’s Mental Health, 2022).
Still, some clinicians advise women to taper or discontinue SSRIs in late pregnancy, but there is not good evidence that this improves neonatal outcomes, which are affected by both treated and untreated mental illness. Importantly, decreasing or discontinuing antidepressants prior to delivery may increase the risk of postpartum depression (MGH Center for Women’s Mental Health, 2022).
Postpartum Hemorrhage
There is some evidence that SSRIs can interfere with platelet function, resulting in bleeding, and there does appear to be an association between SSRIs and SNRIs and postpartum hemorrhage, although the quality of evidence is low, and further research is needed (Viswanathan et al., 2021).
Congenital Malformations and Development
Neither SSRIs nor SNRIs are linked to increased risk of birth defects or changes in mental development after adjusting for confounders associated with underlying mental illness (Betcher & Wisner, 2020).
Prenatal exposure to tricyclic antidepressants or fluoxetine has not been shown to impact IQ, language, temperament, mood, or behavioral development in preschoolers (MGH Center for Women’s Mental Health, 2022; Nulman et al., 1997).
When controlling for underlying psychiatric illness, gestational exposure to SSRIs does not appear to increase the risk of autism spectrum disorders (Kobayashi et al., 2016).
Heart Defects
Some studies have demonstrated a link between antenatal SSRI exposure and heart defects, but most did not control for underlying mental illness, and subsequent studies with more appropriate control groups have failed to show the same association, including a study with a sample size over 900,000 (Payne, 2021).
Several meta-analyses have examined associations between antidepressants (SSRIs, sertraline, citalopram, fluoxetine, paroxetine, and TCAs) and cardiac anomalies but used varying inclusion criteria “that did not consistently exclude cardiac anomalies associated with prematurity” and odds ratios ranged from 0.86 to 1.26, with wide confidence intervals crossing the null (Viswanathan et al., 2021).
Lactation
Breastfeeding mothers who need antidepressant medication should generally take one that has worked well for them in the past (Anderson, 2021).
Some consider sertraline and paroxetine the drugs of choice for breastfeeding women that have not previously used antidepressants due to low levels in breast milk, largely undetectable infant serum levels, and few infant adverse effects (Anderson, 2021).
The relative infant dose of sertraline is around 0.5%, and 1-1.5% for paroxetine.
Fluoxetine has a longer half life of 4-6 days and an active metabolite (norfluoxetine) with half life around 7-15 days, which can result in drug accumulation in breastfed infants and infant serum levels up to 59% of maternal levels that decline slowly after stopping breastfeeding or the mother discontinues the medication (Anderson, 2021).
If a mother used fluoxetine during pregnancy, most experts do not recommend switching to a different medication for breastfeeding (Anderson, 2021).
Citalopram and escitalopram have relative infant doses and half-lives in between those of fluoxetine and sertraline or paroxetine; they can also be used in lactation, particularly if the patient is currently stable on either medication or it has been previously helpful (Anderson, 2021).
Avoidance of Paroxetine (Paxil) in Pregnancy
This is controversial, but generally, it seems that exposure to paroxetine is safer than exposure to untreated mental illness (Lasseter, 2022).
If a patient is stable on paroxetine, it is likely reasonable to continue it during pregnancy, especially if there is a history of severe mental illness, high risk of relapse, or other medications have been ineffective.
Some studies have shown increased risk of heart defects, but others have not. The risk of cardiac defects with paroxetine is lower than once thought and has not been borne out in studies controlling for confounders like maternal depression severity (Huybrechts et al., 2014).
As with other antidepressants, there is a higher risk of neonatal adaptation syndrome, but this is usually mild and of short duration (Payne, 2021).
Similar to other SSRIs, paroxetine is only found in small amounts in breastmilk, and no significant adverse effects have been reported due to exposure to paroxetine through breastfeeding (LactMed, 2022b).
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
Congenital Malformations
Prospective data shows exposure to venlafaxine (Effexor) during the first trimester does not increase risk of major malformations (MGH Center for Women’s Mental Health, 2022).
There is insufficient data about duloxetine (Cymbalta) (MGH Center for Women’s Mental Health, 2022).
As with SSRIs, prenatal exposure to SNRIs is not associated with increased risk of birth defects or changes in mental development after adjusting for confounders associated with underlying mental illness (Betcher & Wisner, 2020).
Lactation
Although research is limited, there have not been reported adverse effects on breastfed infants with duloxetine, and breastmilk levels are very low with a relative infant dose under 1% (Anderson, 2021).
Venlafaxine has an active metabolite (desvenlafaxine) with a longer half life, and the relative infant dose for both substances is ~6.5%, with breastfed infant serum levels ranging from undetectable to 37% of maternal levels; there have been reports of drowsiness or agitation in exposed infants, but most do well, and venlafaxine can be used with caution in lactation (Anderson, 2021).
Bupropion (Wellbutrin)
Congenital Malformations
Bupropion use in pregnancy has not been associated with major malformations (Payne, 2021).
Older reports showed increased rates of heart and great vessel malformation with infants exposed to bupropion, but a retrospective cohort study of 1200 infants with bupropion exposure did not show increased risk of cardiovascular malformations, and the Bupropion Pregnancy Registry data shows rates of congenital malformation (3.9%) similar to those with no known teratogen exposure (MGH Center for Women’s Mental Health, 2022).
Lactation
Bupropion can be used with caution in breastfeeding patients, but there is limited data on its use in lactation, and there have been case reports of possible seizures in breastfed infants, so other medications may be preferred, especially with newborns or premature infants (LactMed, 2023a).
Tricyclic Antidepressants (TCAs)
Of the TCAs, desipramine and nortriptyline are preferred in pregnancy as they are less anticholinergic and may reduce the risk of orthostatic hypotension, which is common in pregnancy (MGH Center for Women’s Mental Health, 2022).
Congenital Malformations
Most studies on tricyclic antidepressants have not found an increased risk of malformations (Payne, 2021).
Lactation
Amitriptyline has been associated with extreme drowsiness in a breastfed infant, although other infants have tolerated exposure to this medication well (Anderson, 2021).
Nortriptyline is an active metabolite of amitriptyline but seems to have fewer adverse effects and does not have any active metabolites of its own, so some consider nortriptyline a drug of choice (along with sertraline and paroxetine) in breastfeeding women that have not previously tried antidepressants (Anderson, 2021).
Doxepin should be avoided in breastfeeding due to reports of serious infant adverse effects (Anderson, 2021).
Monoamine Oxidase Inhibitors (MAOIs)
Pregnancy
MAOIs are usually avoided during pregnancy, as they can lead to hypertensive crises if combined with tocolytic medications like terbutaline, and their use in pregnancy has not been well studied (MGH Center for Women’s Mental Health, 2022).
Lactation
Most MAOIs should be avoided in lactation (Anderson, 2021).
Other Antidepressants
In a prospective study, none of nefazodone, trazodone, and mirtazapine increased rates of congenital malformation (MGH Center for Women’s Mental Health, 2022).
Brexanolone (Zulresso)
Allopregnanolone
Allopregnanolone is a naturally occurring neuroactive progesterone metabolite and GABA-A receptor modulator; when used as a medication, the synthetic analogue of allopregnanolone is called brexanolone (Standeven et al., 2022).
Standeven et al. (2022) report that women with more peripartum mood and anxiety symptoms had lower levels of allopregnanolone in the second trimester (although this was not statistically significant) and higher levels of allopregnanolone at 6 weeks postpartum; these trends persisted whether patients had a psychiatric history or not.
Use in Perinatal Depression
An intravenous preparation of brexanolone (brand name Zulresso) was approved in March 2019 by the FDA and is the first drug specifically designed for postpartum depression (Mughal et al., 2022).
It is only recommended for those with severe postpartum depression whose symptoms are refractory or who decline treatment with antidepressants or ECT (Mughal et al., 2022).
Brexanolone has limited availability and requires continuous monitoring for adverse effects like sedation, loss of consciousness, and hypoxia during a 60 hour infusion (Mughal et al., 2022).
Brexanolone increased the risk of sedation or somnolence to 5%, compared to 0% in the placebo group (Viswanathan et al., 2021).
The long-term safety and efficacy still need to be examined (Mughal et al., 2022).
Efficacy
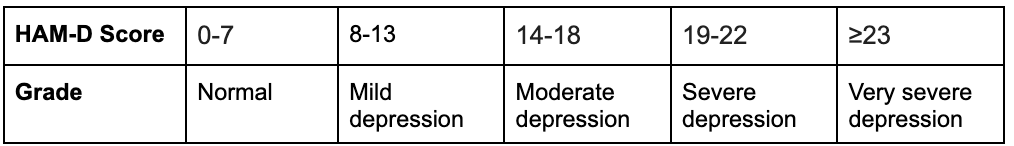
Based on 3 RCTs on brexanolone in a total of 209 women with postpartum depression, the least square mean Hamilton Rating Scale for Depression (HAM-D) scores improved 4.1 points more than placebo at 60 hours and 2.6 points over placebo at 30 days, both of which were statistically significant (Viswanathan et al., 2021).
Given that the Hamilton Rating Scale for Depression (HAM-D) total scores range from 0 to 50, the clinical significance of a 4.1 point improvement can depend on the individual judgment of the treating physician to weigh this potential improvement in the context of other factors, including potential side effects, cost-effectiveness, and feasibility of the treatment regimen.
Table adapted from MDCalc (n.d.) based on the Hamilton Rating Scale for Depression (1960)
Anxiolytics
Benzodiazepines
Due to limited data, the neurodevelopmental effects of prenatal exposure to benzodiazepines remain uncertain (Wang et al., 2022).
Based on the findings of 2 meta-analyses, 2 registry-based studies, and 2 large retrospective cohort studies, pre-pregnancy or prenatal use of benzodiazepines and z-hypnotics is associated with multiple adverse outcomes (Andrade, 2023):
The meta-analyses reported increased rates of spontaneous abortion, induced abortion, preterm birth, low birth weight, small for gestational age, low 5-minute Apgar scores, and neonatal intensive care unit (NICU) admission associated with benzodiazepine and/or z-hypnotic use in pregnancy (Grigoriadis et al., 2020, 2022).
One of the large cohort studies found an increased risk of ectopic pregnancy with benzodiazepine use in the 90 days prior to conception (Wall-Wieler et al., 2020).
The other large cohort study by Noh et al. (2022) found a small but statistically significant increase in risk of overall congenital malformations and cardiac malformations in a South Korean nationwide sample.
In contrast, the two registry studies (Lee et al., 2022; Spuznar et al., 2022) and 2022 meta-analysis by Grigoriadis et al., as well as a previous meta-analysis (Grigoriadis et al., 2019), did not find an increased risk of congenital malformations.
However, it is unclear to what degree these associations result directly from medication exposure, as opposed to possible confounding by indication, confounding by severity of indication, or residual confounding (Andrade, 2023).
Lactation
Medications with antihistamine properties like hydroxyzine and diphenhydramine could decrease breastmilk supply, especially with prolonged use, larger doses, in combination with sympathomimetics like pseudoephedrine, or before breastfeeding is well-established (LactMed, 2021a, 2021b).
Benzodiazepines can be used in lactation, but infants should be monitored for sedation and problems with feeding or growth (LactMed, 2022g, 2023b, 2023c).
Lorazepam has a shorter half-life than many benzodiazepines thus is preferred over other drugs with longer half-lives, like alprazolam and clonazepam (LactMed, 2022g, 2023b, 2023c).
Mood Stabilizers and Anti-epileptic drugs (AEDs)
There are more studies looking at these medications used for epilepsy in pregnancy, not directly investigating psychiatric indications like bipolar disorder.
Payne (2021) recommends encouraging all pregnant women taking anticonvulsants to take high-dose folate (4 mg per day), which can theoretically decrease the risk of neural tube defects.
Valproic acid and carbamazepine should be avoided in pregnancy but can be used in lactation (Payne, 2021).
Avoid Valproic Acid, Valproate, and Divalproex (Depakote) in Women of Childbearing Potential
The most important psychiatric medications to avoid in pregnancy are valproic acid and its derivatives:
Valproate is the conjugate base of valproic acid (National Center for Biotechnology Information, 2023b).
Divalproex is a combination of valproic acid and valproate (National Center for Biotechnology Information, 2023a).
In general, do not prescribe these medications to women of childbearing potential, even if not planning pregnancy in the near future.
However, if a nursing mother requires valproic acid treatment, breastfeeding does appear to be safe (LactMed, 2022k).
Congenital Malformations
A 2021 review by Kaplan and Demir reported estimates of major congenital malformations associated with prenatal valproate/valproic acid exposure ranging from 6.2% to 17.4%, and rates of major congenital malformations were ~2-5 times higher compared to control groups.
The risk of neural tube defects (particularly spina bifida) is approximately 1-2%, which is 10-20 times higher than in the general population (Kaplan & Demir, 2021).
With a neural tube defect risk around 1-6%, valproic acid should only be used as a last resort in women of child-bearing potential due to the high risk of teratogenicity early in pregnancy, often before a woman may be aware of the pregnancy (MGH Center for Women’s Mental Health, 2022).
Effects on Development, Autism, and Intellectual Disability
The effects of prenatal exposure to valproic acid seem to be dose-dependent and are apparent as early as infancy, with lower developmental quotient (DQ) compared to controls (Bromley & Baker, 2017).
Lower intelligence quotient (IQ) in school children, impaired language functioning, memory, social skills, and motor development have also been reported, in addition to increased risk of neurodevelopmental disorders (Bromley & Baker, 2017).
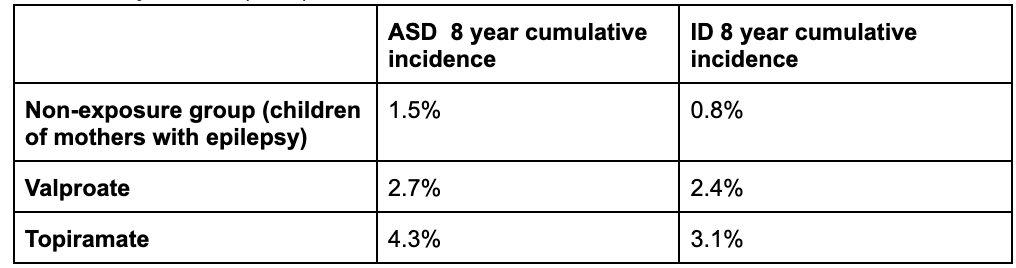
A population-based cohort study with nearly 4.5 million participants looked at rates of autism and intellectual disability in children born to mothers with epilepsy and found that in those who were not exposed to AEDs, 1.5% were diagnosed with autism spectrum disorder (ASD), and 0.8% were diagnosed with intellectual disability by age 8 years (Bjørk et al., 2022).
In same-aged children of mothers with epilepsy exposed to valproate monotherapy, 2.7% had a diagnosis of ASD, and 2.4% were diagnosed with intellectual disability (Bjørk et al., 2022).
4.3% of those exposed to topiramate had ASD, and 3.1% had intellectual disability (Bjørk et al., 2022).
There was no consistently elevated risk of neurodevelopmental disorders associated with prenatal exposure to monotherapy with lamotrigine, carbamazepine, oxcarbazepine, gabapentin, pregabalin, clonazepam, levetiracetam, or phenobarbital (Bjørk et al., 2022).
Data from Bjørk et al. (2022):
ASD: autism spectrum disorders; ID: intellectual disability
Lactation
Although it is contraindicated in pregnancy, valproic acid can be used in lactation, and there do not seem to be adverse effects on growth or development in breastfed infants (LactMed, 2022k). There is very little data specifically on divalproex, although it is rapidly metabolized to valproic acid (LactMed, 2022h).
In fact, one study on children of mothers with epilepsy treated with anti-epileptic drugs (AED) in pregnancy found lower IQ at age 6 associated with prenatal valproate exposure but no adverse effects on IQ with breastmilk exposure to the studied drugs, valproate, carbamazepine, lamotrigine, and phenytoin (Meador et al., 2014).
In children exposed to the studied AEDs, the adjusted mean IQ was 4 points higher in those who were breastfed than those who did not; for children exposed to valproate, adjusted mean IQ was 12 points higher in the breastfed group than the non-breastfed group (Meador et al., 2014).
Valproic acid is excreted at low levels in breastmilk, and infant blood levels are low to undetectable (LactMed, 2022k).
There is a theoretical risk of hepatotoxicity in breastfed infants, so they should be monitored for signs of liver injury like jaundice, although there have been no reported cases (LactMed, 2022k).
Avoid Carbamazepine (Tegretol) in Pregnancy
Carbamazepine use in pregnancy is associated with increased risk of congenital malformations, including neural tube defects, craniofacial abnormalities, skeletal disorders, hypospadias, and diaphragmatic hernia; it may also increase the risk of hemorrhage in the newborn (Payne, 2021).
However, carbamazepine can be used in breastfeeding (LactMed, 2022d; Payne, 2021).
Lamotrigine (Lamictal)
Pregnancy
There is no significantly increased risk of major congenital malformations in babies with prenatal lamotrigine exposure (Kaplan & Demir, 2021).
Analyses of a North American pregnancy registry indicated an increased risk of oral clefts in babies exposed to lamotrigine prenatally, but other registries failed to demonstrate similar findings (Kaplan & Demir, 2021).
When used for seizures, the dose is often increased in pregnancy based on blood levels, but there is not clear evidence that blood levels are correlated with risk of relapse when used for bipolar disorder (MGH Center for Women’s Mental Health, 2020).
It is best to check a lamotrigine level prior to pregnancy in a stable patient so you have a reference point for where to aim in pregnancy if their symptoms relapse (MGH Center for Women’s Mental Health, 2020).
Recheck lamotrigine blood levels within the first 1-2 weeks postpartum, as they can increase after delivery, and the dosage may need to be adjusted, especially if it was increased significantly in pregnancy (MGH Center for Women’s Mental Health, 2020).
Lactation
There do not appear to be adverse effects from lamotrigine monotherapy on growth or development in breastfed infants (LactMed, 2022e).
Toxicity in breastfed infants is rare, but babies should be monitored for apnea, sedation, and poor sucking, as well as rash (LactMed, 2022e)
Transient rashes have been reported in breastfeeding infants exposed to lamotrigine, and there is a theoretical risk of Stevens Johnson Syndrome (SJS), but there have been no reported cases of SJS (Khan et al., 2016).
Infant serum levels should be checked if there is concern for toxicity, and some recommend checking the infant’s serum lamotrigine level, as well as platelets and liver function tests if the maternal dose is increased (LactMed, 2022e).
Lithium
Blood Levels
Lithium has a narrow therapeutic index, and it is important to closely monitor blood levels throughout pregnancy and delivery (Khan et al., 2016).
Lithium dose often needs to be increased during pregnancy due to increased renal clearance and expanded maternal fluid volume, and it should be decreased after delivery as renal clearance and fluid volume begin to normalize postpartum (Khan et al., 2016).
In order to minimize the serum concentration in infants, some recommend stopping lithium at the beginning of labor or 24-48 hours prior to scheduled Cesarean delivery, then restarting the pre-pregnancy dose after delivery (LactMed, 2022m). However, Dr. Lasseter generally recommends against doing so because postpartum psychosis can develop within days after birth, and lithium protects against this. Bergink and Kushner (2014) also advise that discontinuing lithium before delivery is unnecessary as long as maternal blood levels are in the therapeutic range.
Ebstein’s Anomaly
Prenatal lithium exposure, particularly in the first trimester, has been associated with heart defects, but the risk is lower than initially reported; more recent studies estimate the absolute risk of Ebstein’s anomaly to be between 1 in 2000 and 1 in 1000 (0.05-0.1%) (MGH Center for Women’s Mental Health, 2022).
Although there seems to be a small increase in cardiac malformations with lithium, it may be reasonable to start or continue it in pregnancy, especially in women with severe bipolar disorder, in whom the risk of relapse may outweigh the risk of Ebstein’s anomaly (Payne, 2021).
Lactation
Some recommend avoiding lithium in lactation due to high levels of excretion into breast milk. However, according to many sources, lithium use is not an absolute contraindication to breastfeeding, particularly with lithium monotherapy and in healthy, full-term infants, especially those older than 2 months (LactMed, 2022m).
When using lithium in breastfeeding patients, the baby should be monitored for signs of toxicity like feeding difficulties, sedation, restlessness, or poor growth; some groups recommend monitoring infant blood levels at different intervals, while other groups recommend checking lithium levels only when there is a clinical suspicion for toxicity (LactMed, 2022m).
Antipsychotics
Although there is limited data, most antipsychotics appear to be relatively safe in pregnancy, with the exception of risperidone, which is associated with a small increase in congenital malformations (Payne, 2021).
Additionally, postpartum psychosis, in particular, can have devastating consequences, including infanticide, so the benefits of antipsychotic treatment likely outweigh medication risks in patients with serious mental illness (Payne, 2021).
Olanzapine (Zyprexa)
Olanzapine is associated with increased risk of gestational diabetes (Betcher & Wisner, 2020).
Preliminary data from the Massachusetts General Hospital National Pregnancy Registry for Psychiatric Medications show no major congenital malformations associated with first trimester olanzapine exposure in a small sample of 49 infants (Viguera et al., 2023).
There have been reports of sedation in breastfed infants exposed to olanzapine, but overall, it is considered a first-line agent among second-generation antipsychotics in lactation (LactMed, 2022i).
Quetiapine (Seroquel)
Based on four controlled studies, the pooled risk ratio for major malformations in infants with prenatal quetiapine exposure is estimated to be 1.03 (95% CI=0.89, 1.19), suggesting no increased risk (Cohen et al., 2018).
Quetiapine is associated with increased risk of gestational diabetes (Betcher & Wisner, 2020).
Breastmilk levels are low (<1% of the maternal weight-adjusted dose), and based on systematic reviews, quetiapine seems to be the first or second choice among second-generation antipsychotics in lactation (LactMed, 2022j).
Aripiprazole (Abilify)
Among 163 infants exposed to aripiprazole in the first trimester, the risk of major malformations was not different compared to controls after adjusting for confounding variables (Freeman et al., 2021).
Data on lactation is limited, and other medications with more data may be preferred over aripiprazole, especially if breastfeeding a newborn or premature infant (LactMed, 2022l).
There have been reports of gynecomastia, galactorrhea, and cessation of lactation, in addition to impaired growth and weight loss in breastfed infants (LactMed, 2022l).
Risperidone (Risperdal)
Risperidone (and potentially paliperidone) seems to increase the risk of overall and cardiac malformations (Betcher & Wisner, 2020).
Risperidone may be considered as a second-line antipsychotic and used cautiously in lactation, but other agents are preferred due to higher breastmilk levels than other medications and reports of “Sedation, failure to thrive, jitteriness, tremors and abnormal muscle movements” in breastfed infants (LactMed, 2023e).
Clozapine (Clozaril)
Clozapine does not appear to be teratogenic, although data is limited (Beex-Oosterhuis et al., 2021).
Clozapine use in pregnancy is associated with 2x higher rates of gestational diabetes and may increase the risk of floppy infant syndrome and neonatal seizures (Mehta & Van Lieshout, 2017).
Several sources recommend against breastfeeding when taking clozapine due to risks of sedation and agranulocytosis in the infant (LactMed, 2022a).
Lactation
Data on antipsychotics and lactation is limited, but a 2016 systematic review of 37 reports found that second generation antipsychotics appear to be relatively safe in lactation, with the exception of clozapine (Uguz, 2016).
Antipsychotics can cause hyperprolactinemia and resulting galactorrhea (milk production in men or nonpregnant, nonlactating women) due to dopamine blockade in the tuberoinfundibular pathway; this has been reported in several different medications, including haloperidol and risperidone (LactMed, 2022f, 2023e).
Galactorrhea has also been reported in olanzapine, quetiapine, and aripiprazole, although these medications have a minimal effect on serum prolactin levels (LactMed, 2022i, 2022j, 2022l).
In nursing mothers with established lactation, the effects of these antipsychotics on prolactin levels may not interfere with breastfeeding (LactMed, 2022f, 2022i, 2022j, 2022l, 2023e).
There have also been case reports of aripiprazole associated with decreased breast milk supply (LactMed, 2022l).
Substance Use Disorders
An estimated 1-5% of pregnancies worldwide are affected by substance use disorders (Nagpal et al., 2020).
A 2013 national survey reported that in the United States, 15.4% of pregnancies were exposed to cigarettes, 9.4% to alcohol, and 5.4% to illicit substances (Louw, 2018).
Substance abuse causes many adverse effects in pregnancy and beyond, including fetal toxicity or teratogenicity, and overdose, which can sadly result in death and other devastating consequences.
Pregnancy motivates many women to stop using, decrease use, or seek out substance use treatment, but some are unable to quit during pregnancy due to the chronic, relapsing nature of these disorders (Louw, 2018).
Unfortunately, postpartum relapse rates are high, particularly in the first 6 months; one prospective study on substance use in pregnant women found that 83% were able to achieve abstinence from at least one substance, but 80% relapsed with at least one substance postpartum (Louw, 2018).
Although criminalization does not lead to better outcomes for either mother or child, some states mandate reporting of all substance use in pregnancy to Child Protective Services (CPS), including prescriptions and medication-assisted treatment, and it is considered child abuse in 18 US states (Prince et al., 2023).
Prenatal substance use is also grounds for involuntary commitment in 3 states (Prince et al., 2023).
Many women avoid prenatal care or hide substance use from their care team due to fear of consequences like losing custody or being arrested (Prince et al., 2023).
It is vital that we support our patients and adequately treat their substance use disorders before, during, and after pregnancy, practicing harm reduction when applicable.
Harm Reduction
See the Pregnancy and Substance Use: A Harm Reduction Toolkit from the CDC
Alcohol
Fetal Alcohol Spectrum Disorders
Alcohol is a well-known teratogen and can cause fetal alcohol spectrum disorders, which include a variety of adverse effects on physical, neurological, and behavioral development (Chung et al., 2021).
In the United States, fetal alcohol syndrome is the most common cause of preventable intellectual disability (Prince et al., 2023).
Naltrexone and Acamprosate
While there is little data on the safety of alcohol use disorder medications in pregnancy, acamprosate and naltrexone have not been associated with significant risks of congenital malformation or other serious adverse effects and should be considered in pregnancy given the known risks of alcohol consumption (Kelty et al., 2021).
Disulfiram
Disulfiram should be avoided in pregnancy due to evidence (albeit limited) of adverse effects from clinical and animal studies (Kelty et al., 2021).
Opioids
Neonatal Opioid Withdrawal Syndrome (NOWS)
Prenatal opioid exposure can lead to neonatal opioid withdrawal syndrome (NOWS), which is associated with neurological, gastrointestinal, and respiratory adverse effects and may require prolonged hospitalization (Prince et al., 2023).
Methadone and Buprenorphine
Methadone and buprenorphine are considered safe in pregnancy and can be used in lactation (Nagpal et al., 2020).
Note that this is buprenorphine without naloxone—the combination of buprenorphine and naloxone is suboxone, which is not recommended.
Stimulants
Prescribed Stimulants vs Stimulants of Abuse
It is important to make the distinction between prescribed stimulant use (e.g., for ADHD treatment) versus substance abuse, which generally involves much higher doses and can have more severe effects on offspring.
For example, prenatal methamphetamine use is associated with fetal growth restriction and low birth weight (Sankaran et al., 2022), as well as widespread effects on brain development and impairments in intellectual functioning, problem solving, short-term memory, and language development (Kunkler et al., 2022).
Attention-Deficit/Hyperactivity Disorder (ADHD)
In patients with moderate to severe functional impairment, the benefits can outweigh risks of stimulant medication, such as improving safety while driving (Baker & Freeman, 2018).
Methylphenidate
Methylphenidate has been the best studied, and most studies on stimulants used for ADHD in pregnancy have not found an association with malformations (Baker & Freeman, 2018).
While some studies have found associations with prenatal exposure to stimulants and outcomes like miscarriage, low birth weight, placental problems, and low Apgar scores, others have found no change in risk for congenital malformations, prematurity, or birth weight (Baker & Freeman, 2018).
It is possible that some of the adverse outcomes associated with these medications may be related to the underlying mental illness, rather than the medication alone (Baker & Freeman, 2018).
Mothers who require methylphenidate can continue breastfeeding (LactMed, 2023d).
Lactation
Methylphenidate is undetectable in the serum of breastfed infants, and breastmilk levels appear to be very low, around 0.16%–0.7% of the maternal weight-adjusted dose (LactMed, 2023d).
In typically-prescribed doses, dextroamphetamine does not appear to have adverse effects on nursing infants, and the breastfed infant dosage also seems to be relatively low: 5.7% of maternal dose in one study (Baker & Freeman, 2018).
Tobacco
Behavioral Interventions
Counseling (e.g., motivational interviewing or cognitive behavioral therapy) and financial incentives are associated with decreased rates of smoking in pregnancy and lower risk of low birth weight (American College of Obstetricians and Gynecologists’ [ACOG] Committee on Obstetric Practice et al., 2020).
Bupropion (Wellbutrin; Zyban)
Although data is limited, bupropion use in pregnancy is not associated with known risks of fetal anomalies, low birth weight, or preterm birth (ACOG Committee on Obstetric Practice et al., 2020).
Bupropion can be used with caution in breastfeeding patients, but there is limited data on its use in lactation, and there have been case reports of possible seizures in breastfed infants, so other medications may be preferred, especially with newborns or premature infants (LactMed, 2023a).
Varenicline (Chantix)
Data on varenicline are very limited, but some small studies have not found evidence of teratogenicity (ACOG Committee on Obstetric Practice et al., 2020).
Varenicline is not recommended in breastfeeding due to a lack of evidence, whereas the safety of bupropion in lactation has been somewhat better established (ACOG Committee on Obstetric Practice et al., 2020).
Nicotine Replacement Therapy
While some reviews support the efficacy of nicotine replacement for smoking cessation in pregnancy, the evidence is inconsistent, and several US trials have been stopped early due to adverse effects or ineffectiveness (ACOG Committee on Obstetric Practice et al., 2020).
Nicotine replacement therapy should only be considered in pregnancy with close monitoring and after detailed discussion of the known risks of continuing to smoke and the possible risks of nicotine replacement (ACOG Committee on Obstetric Practice et al., 2020).
The authors of the LactMed® chapter on nicotine advise avoiding all forms of nicotine in nursing mothers (LactMed, 2020).
The equivalent amount of nicotine from 17 cigarettes passes into the milk daily in breastfeeding mothers using a 21 mg transdermal nicotine patch (LactMed, 2020).
Some advocate for smoking mothers using nicotine replacement in order to reduce breastfed infant exposure to smoke and toxins from cigarettes; however, animal data suggests that nicotine could interfere with infant lung development and may increase the risk of sudden infant death syndrome (SIDS) (LactMed, 2020).
Marijuana And Cannabinoids (CBD, THC, Delta-8, etc.)
The use of marijuana and cannabinoids in the perinatal period seems to be increasing in the setting of more widespread legalization and availability (Martin, 2020).
Cannabinoids have been shown to affect pregnancy through activating the endocannabinoid system, including CB1 and CB2 receptors (Martin, 2020).
Perinatal cannabinoid use is associated with impairments in offspring behavioral, cognitive, and emotional development (Martin, 2020).
Although there is no definitive data, marijuana has been associated with preterm birth, low birth weight, and stillbirth (Prince et al., 2023).
The ACOG recommends avoiding marijuana in pregnancy, and the AAP recommends that mothers using marijuana should not breastfeed (Martin, 2020).
Perinatal Psychotherapy
Depression
Most research on perinatal psychotherapy has studied patients with major depression or depressive symptoms and indicates that psychotherapy is a safe and effective treatment for perinatal depression.
Psychological interventions such as therapy should be considered first-line treatment for perinatal depression (Cuijpers & Karyotaki, 2021).
Cuijpers and Karyotaki (2021) found that psychological interventions were effective in treating perinatal depression, which remained significant at 12 months after treatment initiation, with an effect size of g=0.67 and number needed to treat (NNT) around 4.
Although therapy may be less effective in patients with chronic depression, psychological interventions are effective, particularly in subthreshold depression where they may prevent progression to major depression (Cuijpers & Karyotaki, 2021).
Meta-analysis by Jiang et al. (2022) with 21 included RCTs found significant improvements in perinatal depression from cognitive behavioral therapy (CBT) and interpersonal therapy (IPT); IPT was more effective than CBT, and brief interpersonal therapy (IPT-B) was better than standard IPT.
In a prospective randomized clinical trial of pregnant patients from diverse backgrounds with major depressive disorder, IPT-B led to significant improvement in depressive symptoms compared to enhanced usual care (Hankin et al., 2023).
Fatherhood and Mental Health
Although it is frequently underrecognized, misdiagnosed, and undertreated, the prevalence of paternal postpartum depression is estimated between 1.2% and 25.5% and is associated with paternal unemployment and psychological status, maternal mental illness, first pregnancy, and quality of marital relationship (Wang et al., 2021).
In addition to the lack of awareness and screening for paternal mental illness, men with perinatal depression are more likely than women to present with anger, irritability, or interpersonal conflict, which can lead to misdiagnosis (Skilbeck et al., 2023).
Risks of Paternal Perinatal Depression
Paternal perinatal depression is correlated with maternal perinatal depression (Skilbeck et al., 2023).
Additionally, Ashraf et al. (2023) reports that poor paternal mental health, particularly depression, at any stage of child development is associated with a broad range of negative impacts on children, including:
Increased distress in infants and impaired socioemotional development
Disruptive behavior, including oppositional defiant disorder (ODD), conduct disorder (CD), and attention-deficit/hyperactivity disorder (ADHD)
Neurodevelopmental disorders, such as increased rates of autism spectrum disorders (ASD)
Impaired speech and language development
“Hostile home environments and dysfunctional family dynamics”
Low income, which can further impact maternal and infant health
Benefits of Involved Fathers
Paternal involvement is associated with better early infant neurodevelopment, and this effect is partially mediated by a resulting reduction of parenting stress in mothers (Kim et al., 2016).
Research also shows that supportive fathers can help moderate the effects of maternal adverse childhood experiences (ACEs) on prenatal depressive symptoms, although mothers with high ACE scores are still at increased risk of prenatal depressive symptoms despite high paternal support (Fields et al., 2022).
A prospective study of 95 pregnant women found that involvement of the father of the baby was associated with decreased depressive symptoms and better psychological well-being (Giurgescu & Templin, 2015).
A Japanese cohort study of over 18,000 children found that more active paternal involvement in childcare tasks (like changing diapers) at 6 months of age was associated with greater psychological well-being at 16 years old (Kato et al., 2023).
Treatment of Paternal Mental Illness
While there is limited evidence about treatment of perinatal mental health treatment of fathers, one case study by Skilbeck et al. (2023) reports significant improvement of paternal perinatal depression symptoms in a 22-year-old first-time father taking 20 mg citalopram after attending 12 weekly sessions of cognitive behavioral therapy (CBT) over 4 months, with maintenance at 3-month follow-up:
Data from Skilbeck et al. (2023)
See also: Raising An Emotionally Intelligent Child
Exercise
Effects on Perinatal Depression and Anxiety
High levels of physical activity during pregnancy are associated with lower risk of prenatal depression and anxiety, as well as decreased severity of prenatal depression and anxiety symptoms, reduced stress, and increased quality of life, although pre-pregnancy physical activity did not affect these outcomes (Cai et al., 2022).
In addition to decreased postnatal depression and anxiety, prenatal exercise is associated with enhanced placental growth and nutrient transport during pregnancy (Nagpal et al., 2020).
Levels of BDNF increase in response to exercise, including in pregnant women, and this is thought to mediate at least some of the positive effects of exercise on mental health (Nagpal et al., 2020).
Exercise-based and physical activity interventions may be helpful in the prevention or treatment of perinatal depression, though more rigorous research is needed (Carter et al., 2019).
Among 18 trials on exercise for postpartum depression, overall quality of evidence was low, and there were small effect sizes of exercise interventions (mostly aerobic exercise and coaching vs. usual care) decreasing depressive symptoms (Carter et al., 2019).
Meta-analysis of 12 RCTs found an effect size of 0.41 of perinatal physical activity interventions on postpartum depressive symptoms; with subgroup analysis, they found effect sizes of 0.67 in patients who met postpartum depression criteria at baseline and 0.29 for those who did not meet this criteria (Poyatos-León et al., 2017).
Exercise and Substance Use Disorders
According to Nagpal et al. (2020):
There is some evidence for exercise as an adjunctive treatment for substance use disorder, but insufficient data in pregnancy specifically.
Some of this effect may be due to exercise-related stress reduction and mood improvement, which reduces risk of relapse.
Animal studies with morphine-dependent pregnant rats have found that exercise was associated with decreased anxiety-related behaviors in the mothers during withdrawal.
The pups of morphine-dependent mothers who exercised showed decreased anxiety, decreased voluntary morphine consumption, and increased BDNF in the bone marrow stromal cells compared to pups with sedentary mothers.
Yoga
Meta-analysis by Jiang et al. (2022) found no significant effect of yoga on perinatal depression.
However, some studies have found improvements in depression and anxiety symptoms with perinatal yoga (Muzik et al., 2012; Battle et al., 2015).
A systematic review of 13 studies found evidence for the efficacy of yoga interventions on decreasing depression and anxiety symptoms in pregnant women, although 7 of the 13 also incorporated mindfulness and/or meditation in the intervention (Sheffield & Woods-Giscombé, 2016).
Overall, more research is needed, and there is not strong evidence for the benefits of yoga in this population.
However, yoga is difficult to study due to the heterogeneity of different practices, and it is possible that certain types of yoga are in fact beneficial for perinatal mental health.
Vitamins and Other Nutrients
Omega-3’s/Fish Oil
Mocking et al. (2020) suggest that omega-3 polyunsaturated fatty acids (PUFA) may be an effective adjunctive treatment in postpartum depression, but not for prevention or treatment of depression in pregnancy.
The largest effect of omega-3 PUFA was seen in postpartum depression (-0.886 standardized difference in means [SDM]).
There was a medium to large effect in postpartum women (SDM= -0.656), but negligible effect in pregnancy (SDM= -0.071).
The effect in depressed women was medium (SDM= -0.545), with no effect in women without depression (SDM= -0.073).
Diet
Dietary Effects on Depression
Although there is very little research on diet and perinatal mental health specifically, diet has been shown to impact depression in non-pregnant adults.
The Mediterranean diet appears to result in reduction or remission of depressive symptoms in non-pregnant adults (Ventriglio et al., 2020).
There is also evidence that polyphenols can improve symptoms of depression, and the protective effects of the Mediterranean diet on depression may result from increased consumption of polyphenol-rich foods (e.g., coffee, tea, grapes, citrus, nuts, legumes, and spices) (Bayes et al., 2020).
Prenatal Diet and Offspring Development
Although the results were limited by a large number of animal studies, a 2022 scoping review with 120 included articles found lower rates of offspring anxiety with increased maternal consumption of vitamins and phytochemicals; offspring anxiety rates increased with reduced consumption of omega-3’s and maternal restriction of calories or protein (Monteiro et al., 2022).
A 2017 systematic review and meta-analysis by Borge et al. with 18 studies and over 63,000 participants found small positive associations between better maternal diet and child neurodevelopment.
In the affective domain: Hedge's g=0.088, adjusted for publication bias (unadjusted g=0.093)
Cognitive domain: g=0.14 (no publication bias observed)
Overall summary effect size: g=0.075, adjusted for publication bias (unadjusted g=0.112)
Prenatal Vitamins
A 2019 systematic review and meta-analysis found lower rates of offspring autism spectrum disorders (ASD) with maternal prenatal folic acid or multivitamin use (Li et al., 2019).
In a study of 418 mother-child dyads, moderate-to-severe depression was associated with impaired offspring cognition at 4 years old, and this finding persisted regardless of maternal prenatal vitamin intake (Ssewanyana et al., 2022).
Folate
Folate is commonly used in women of childbearing potential to reduce the risk of neural tube defects, and there is some evidence for its use as an adjunctive treatment in perinatal depression (Deligiannidis & Freeman, 2014).
Vitamin D
The current evidence on the relationship between vitamin D and perinatal depression is inconclusive due to poor study quality and heterogeneity (Gould et al., 2022).
However, there is evidence that maternal vitamin D deficiency increases the risk of offspring attention-deficit/hyperactivity disorder and autism spectrum disorder in a dose-dependent manner (Tirani et al., 2023; Upadhyaya et al., 2022).
It is also hypothesized that prenatal exposure to vitamin D deficiency increases the risk of schizophrenia based on higher rates of schizophrenia in people born in winter or spring and “offspring of dark-skinned migrants living in cold climates,” both of which are associated with vitamin D deficiency (Albiñana et al., 2022).
There is some data showing an association between neonatal vitamin deficiency and schizophrenia, though it is possible vitamin D supplementation may not actually mitigate this risk, as common genetic variants linked to schizophrenia also lead to lower vitamin D levels (Albiñana et al., 2022).
Vitamin B12
There is not convincing evidence that vitamin B12 deficiency is associated with either depression in pregnancy or restless leg syndrome (Ramadan et al., 2022).
Complementary And Alternative Medicine
The peripartum period is a vulnerable time, and there are many fads that promise to provide benefit, but may truly be only a placebo or could potentially cause harm.
Many patients prefer alternative non-pharmacologic treatments for peripartum depression due to concern about potential adverse effects on the fetus or infant and may seek Complementary and Alternative Medicine (CAM) treatments (Deligiannidis & Freeman, 2014).
A national survey in 2007 found that nearly 40% of American adults had used CAM in the past month (Barnes et al., 2008).
Placentophagy
The practice of placentophagy, or consuming the placenta after childbirth, is becoming more popular in Western societies among certain groups of women based on the belief that it can improve mood, increase lactation, and aid recovery by replenishing lost nutrients and hormones (Marraccini & Gorman, 2015).
Placentophagy is common among mammals, and animal studies have demonstrated positive influences on maternal behavior and pain (Marraccini & Gorman, 2015).
However, there is no empirical evidence to support these claims in humans, and further research is needed to establish the properties of the human placenta, effects of encapsulation, and potential benefits or harms of consuming it (Marraccini & Gorman, 2015).
St John's Wort (hypericum perforatum)
There is some evidence that St John’s wort has efficacy similar to TCAs or SSRIs in mild to moderate depression compared to placebo (Deligiannidis & Freeman, 2014).
However, it is not recommended in pregnant patients due to safety concerns including numerous medication interactions, lack of regulation or standardized dosing (because it is a supplement, thus not regulated by the FDA), and evidence of adverse effects in studies on breastfed infants, as well as in vitro and animal models (Zepeda et al., 2023).
Bright Light Therapy
There is growing interest in bright light therapy as a treatment for perinatal depression, and light boxes are increasingly commercially available.
A randomized controlled trial by Donmez et al. (2022) found significant improvement in perinatal depression symptoms with 45 minutes of daily bright light therapy (10,000 lux) each morning for 3 weeks.
Response rate in the bright light therapy group was 75%, compared to 18.2% in the placebo light condition (<500 lux).
Remission rate with bright light therapy was 41.7% and 0% with placebo.
Deligiannidis & Freeman (2014) recommend starting with 30 minutes of bright light therapy in the morning within 10 minutes of waking up.
Due to the possibility of undiagnosed bipolar disorder, patients starting bright light therapy should be monitored closely for signs of hypomania, mania, sleep difficulties, or agitation (Deligiannidis & Freeman, 2014).
Massage
There is some evidence that massage therapy can decrease depressive symptoms in pregnant and non-pregnant people, and antenatal massage may reduce rates of prematurity and low birth weight (Deligiannidis & Freeman, 2014).
Massage therapy combined with group psychotherapy has also been shown to reduce antenatal depression symptoms and cortisol levels more than group psychotherapy alone (Deligiannidis & Freeman, 2014).
Acupuncture
A meta-analysis of 30 trials found insufficient evidence for efficacy of acupuncture in major depression compared to sham treatment (Deligiannidis & Freeman, 2014).
Connect with Dr. Kristin Lasseter:
Instagram: the.reproductive.psychiatrist
Private Practice Website: Reproductive Psychiatry & Counseling Austin Texas
You Tube: Medical Mamas
Resources
Perinatal Psychiatry Access Programs
Various states have Perinatal Psychiatry Access Programs that allow clinicians to consult with perinatal psychiatrists about their patients, for example, PeriPAN in Texas. UMass Chan Medical School has a list of programs at the link above.
The Periscope Project Provider Toolkit
Perinatal psychiatry resources for healthcare providers
LactMed®
Drugs and Lactation Database (LactMed®) is a fully-referenced database that provides information about levels of drugs and other substances in breastmilk and infant blood, possible adverse effects on nursing infants, and appropriate therapeutic alternatives.
REPROTOX®
The Reproductive Toxicology Center developed REPROTOX®, a database summarizing “the effects of medications, chemicals, infections, and physical agents on pregnancy, reproduction, and development.”
Pregnancy and Substance Use: A Harm Reduction Toolkit
From the CDC
ACOG
More perinatal mental health resources for providers, patients, and families from ACOG
References:
American College of Obstetricians and Gynecologists’ Committee on Obstetric Practice,
Valent, A., Choby, B. (2020). Tobacco and Nicotine Cessation During Pregnancy:
ACOG Committee Opinion, Number 807. Obstetrics and gynecology, 135(5),
e221–e229. https://doi.org/10.1097/AOG.0000000000003822
Albiñana, C., Boelt, S. G., Cohen, A. S., Zhu, Z., Musliner, K. L., Vilhjálmsson, B. J., &
McGrath, J. J. (2022). Developmental exposure to vitamin D deficiency and
subsequent risk of schizophrenia. Schizophrenia research, 247, 26–32.
https://doi.org/10.1016/j.schres.2021.06.004
Anderson P. O. (2021). Antidepressants and Breastfeeding. Breastfeeding medicine : the
official journal of the Academy of Breastfeeding Medicine, 16(1), 5–7.
https://doi.org/10.1089/bfm.2020.0350
Andrade C. (2022). Gestational Exposure to Antidepressant Drugs and
Neurodevelopment: An Examination of Language, Mathematics, Intelligence, and
Other Cognitive Outcomes. The Journal of clinical psychiatry, 83(1), 22f14388.
https://doi.org/10.4088/JCP.22f14388
Andrade C. (2023). Gestational Exposure to Benzodiazepines and Z-Hypnotics and the Risk
of Major Congenital Malformations, Ectopic Pregnancy, and Other Adverse Pregnancy
Outcomes. The Journal of clinical psychiatry, 84(2), 23f14874.
https://doi.org/10.4088/JCP.23f14874
Ashraf, S., Shah, K., Vadukapuram, R., Shah, B., Jaiswal, S., Mansuri, Z., & Jain, S. (2023).
Impact of Paternal Depression on Child Neurodevelopmental Outcomes and
Disorders. The primary care companion for CNS disorders, 25(1), 22r03303.
https://doi.org/10.4088/PCC.22r03303
Baker, A. S., & Freeman, M. P. (2018). Management of Attention Deficit Hyperactivity Disorder
During Pregnancy. Obstetrics and gynecology clinics of North America, 45(3),
495–509. https://doi.org/10.1016/j.ogc.2018.04.010
Barnes, P. M., Bloom, B., & Nahin, R. L. (2008). Complementary and alternative medicine
use among adults and children: United States, 2007. National health statistics reports,
(12), 1–23.
Battle, C. L., Uebelacker, L. A., Magee, S. R., Sutton, K. A., & Miller, I. W. (2015). Potential
for prenatal yoga to serve as an intervention to treat depression during
pregnancy. Women's health issues : official publication of the Jacobs Institute of
Women's Health, 25(2), 134–141. https://doi.org/10.1016/j.whi.2014.12.003
Bayes, J., Schloss, J., & Sibbritt, D. (2020). Effects of Polyphenols in a Mediterranean
Diet on Symptoms of Depression: A Systematic Literature Review. Advances in
nutrition (Bethesda, Md.), 11(3), 602–615.
https://doi.org/10.1093/advances/nmz117
Beex-Oosterhuis, M. M., Van Gool, A. R., Heerdink, E. R., van Kesteren, C., & van Marum, R.
J. (2021). Clozapine Treatment During Pregnancy and the Postpartum Period: A
Systematic Literature Review. The Journal of clinical psychiatry, 83(1), 21r13952.
https://doi.org/10.4088/JCP.21r13952
Bergink, V., & Kushner, S. A. (2014). Lithium during pregnancy. The American journal of
psychiatry, 171(7), 712–715. https://doi.org/10.1176/appi.ajp.2014.14030409
Betcher, H. K., & Wisner, K. L. (2020). Psychotropic Treatment During Pregnancy:
Research Synthesis and Clinical Care Principles. Journal of women's health
(2002), 29(3), 310–318. https://doi.org/10.1089/jwh.2019.7781
Bjørk, M. H., Zoega, H., Leinonen, M. K., Cohen, J. M., Dreier, J. W., Furu, K., Gilhus, N. E.,
Gissler, M., Hálfdánarson, Ó., Igland, J., Sun, Y., Tomson, T., Alvestad, S., &
Christensen, J. (2022). Association of Prenatal Exposure to Antiseizure
Medication With Risk of Autism and Intellectual Disability. JAMA neurology, 79(7),
672–681. https://doi.org/10.1001/jamaneurol.2022.1269
Borge, T. C., Aase, H., Brantsæter, A. L., & Biele, G. (2017). The importance of maternal
diet quality during pregnancy on cognitive and behavioural outcomes in children:
a systematic review and meta-analysis. BMJ open, 7(9), e016777.
https://doi.org/10.1136/bmjopen-2017-016777
Bromley, R. L., & Baker, G. A. (2017). Fetal antiepileptic drug exposure and cognitive
outcomes. Seizure, 44, 225–231. https://doi.org/10.1016/j.seizure.2016.10.006
Cai, C., Busch, S., Wang, R., Sivak, A., & Davenport, M. H. (2022). Physical activity before
and during pregnancy and maternal mental health: A systematic review and meta-analysis of observational studies. Journal of affective disorders, 309, 393–403. https://doi.org/10.1016/j.jad.2022.04.143
Carter, T., Bastounis, A., Guo, B., & Jane Morrell, C. (2019). The effectiveness of
exercise-based interventions for preventing or treating postpartum depression: a
systematic review and meta-analysis. Archives of women's mental health, 22(1),
37–53. https://doi.org/10.1007/s00737-018-0869-3
Centers for Disease Control and Prevention. (2022, September 19). Four in 5
pregnancy-related deaths in the U.S. are preventable. Centers for Disease Control and
Prevention. Retrieved February 20, 2023, from
https://www.cdc.gov/media/releases/2022/p0919-pregnancy-related-deaths.html
Chung, D. D., Pinson, M. R., Bhenderu, L. S., Lai, M. S., Patel, R. A., & Miranda, R. C.
(2021). Toxic and Teratogenic Effects of Prenatal Alcohol Exposure on Fetal
Development, Adolescence, and Adulthood. International journal of molecular
sciences, 22(16), 8785. https://doi.org/10.3390/ijms22168785
Cohen L.S. (2019). Course and Treatment of Mood Disorders during Pregnancy and the
Postpartum Period: Lessons Learned Across Two Decades [PowerPoint Presentation].
MGH Psychiatry Academy Women’s Mental Health Course.
Cohen, L. S., Góez-Mogollón, L., Sosinsky, A. Z., Savella, G. M., Viguera, A. C., Chitayat, D.,
Hernández-Díaz, S., & Freeman, M. P. (2018). Risk of Major Malformations in Infants
Following First-Trimester Exposure to Quetiapine. The American journal of psychiatry,
175(12), 1225–1231. https://doi.org/10.1176/appi.ajp.2018.18010098
Cuijpers, P., & Karyotaki, E. (2021). The effects of psychological treatment of perinatal
depression: an overview. Archives of women's mental health, 24(5), 801–806.
https://doi.org/10.1007/s00737-021-01159-8
Deligiannidis, K. M., & Freeman, M. P. (2014). Complementary and alternative medicine
therapies for perinatal depression. Best practice & research. Clinical obstetrics &
gynaecology, 28(1), 85–95. https://doi.org/10.1016/j.bpobgyn.2013.08.007
Donmez, M., Yorguner, N., Kora, K., & Topcuoglu, V. (2022). Efficacy of bright light therapy in
perinatal depression: A randomized, double-blind, placebo-controlled study. Journal of
psychiatric research, 149, 315–322. https://doi.org/10.1016/j.jpsychires.2022.02.027
BK501922/
Drugs and Lactation Database (LactMed®). (2020, August 17). Nicotine. National Institute of
Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501586/
Drugs and Lactation Database (LactMed®). (2021a, September 20). Diphenhydramine.
National Institute of Child Health and Human Development. Retrieved June 22, 2023
from https://www.ncbi.nlm.nih.gov/books/NBK501878/
Drugs and Lactation Database (LactMed®). (2021b, September 20). Hydroxyzine. National
Institute of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK500985/
Drugs and Lactation Database (LactMed®). (2022a, May 15). Clozapine. National Institute of
Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501650/
Drugs and Lactation Database (LactMed®). (2022b, May 15). Paroxetine. National Institute of
Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501190/
Drugs and Lactation Database (LactMed®). (2022c, May 15). Sertraline. National Institute of
Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501191/
Drugs and Lactation Database (LactMed®). (2022d, June 20). Carbamazepine. National
Institute of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501271/
Drugs and Lactation Database (LactMed®). (2022e, June 20). Lamotrigine. National Institute
of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501268/
Drugs and Lactation Database (LactMed®). (2022f, July 18). Haloperidol. National Institute of
Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK500910/
Drugs and Lactation Database (LactMed®). (2022g, November 30). Clonazepam. National
Institute of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501209/
Drugs and Lactation Database (LactMed®). (2022h, November 30). Divalproex. National
Institute of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501311/
Drugs and Lactation Database (LactMed®). (2022i, November 30). Olanzapine. National
Institute of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501056/
Drugs and Lactation Database (LactMed®). (2022j, November 30). Quetiapine. National
Institute of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501087/
Drugs and Lactation Database (LactMed®). (2022k, November 30). Valproic Acid. National
Institute of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501274/
Drugs and Lactation Database (LactMed®). (2022l, December 19). Aripiprazole. National
Institute of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501016/
Drugs and Lactation Database (LactMed®). (2022m, December 19). Lithium. National
Institute of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501153/
Drugs and Lactation Database (LactMed®). (2023a, January 15). Bupropion. National
Institute of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501184/
Drugs and Lactation Database (LactMed®). (2023b, February 15). Alprazolam. National
Institute of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501199/
Drugs and Lactation Database (LactMed®). (2023c, February 15). Lorazepam. National
Institute of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501231/
Drugs and Lactation Database (LactMed®). (2023d, February 15). Methylphenidate. National
Institute of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501310/
Drugs and Lactation Database (LactMed®). (2023e, May 15). Risperidone. National Institute
of Child Health and Human Development. Retrieved June 22, 2023 from
https://www.ncbi.nlm.nih.gov/books/NBK501095/
Fields, K., Shreffler, K. M., Ciciolla, L., Baraldi, A. N., & Anderson, M. (2023). Maternal
childhood adversity and prenatal depression: the protective role of father
support. Archives of women's mental health, 26(1), 89–97.
https://doi.org/10.1007/s00737-022-01278-w
Freeman, M. P., Viguera, A. C., Góez-Mogollón, L., Young, A. V., Caplin, P. S., McElheny, S.
A., Church, T. R., Chitayat, D., Hernández-Díaz, S., & Cohen, L. S. (2021).
Reproductive safety of aripiprazole: data from the Massachusetts General Hospital National Pregnancy Registry for Atypical Antipsychotics. Archives of women's mental health, 24(4), 659–667. https://doi.org/10.1007/s00737-021-01115-6
Giurgescu, C., & Templin, T. N. (2015). Father Involvement and Psychological Well-Being of
Pregnant Women. MCN. The American journal of maternal child nursing, 40(6),
381–387. https://doi.org/10.1097/NMC.0000000000000183
Gould, J. F., Gibson, R. A., Green, T. J., & Makrides, M. (2022). A Systematic Review of
Vitamin D during Pregnancy and Postnatally and Symptoms of Depression in the
Antenatal and Postpartum Period from Randomized Controlled Trials and
Observational Studies. Nutrients, 14(11), 2300.
https://doi.org/10.3390/nu14112300
Grigoriadis, S., Alibrahim, A., Mansfield, J. K., Sullovey, A., & Robinson, G. E. (2022).
Hypnotic benzodiazepine receptor agonist exposure during pregnancy and the risk of
congenital malformations and other adverse pregnancy outcomes: A systematic
review and meta-analysis. Acta psychiatrica Scandinavica, 146(4), 312–324.
https://doi.org/10.1111/acps.13441
Grigoriadis, S., Graves, L., Peer, M., Mamisashvili, L., Dennis, C. L., Vigod, S. N., Steiner, M.,
Brown, C., Cheung, A., Dawson, H., Rector, N., Guenette, M., & Richter, M. (2019).
Benzodiazepine Use During Pregnancy Alone or in Combination With an
Antidepressant and Congenital Malformations: Systematic Review and Meta-Analysis.
The Journal of clinical psychiatry, 80(4), 18r12412.
https://doi.org/10.4088/JCP.18r12412
Grigoriadis, S., Graves, L., Peer, M., Mamisashvili, L., Ruthirakuhan, M., Chan, P., Hennawy,
M., Parikh, S., Vigod, S. N., Dennis, C. L., Steiner, M., Brown, C., Cheung, A.,
Dawson, H., Rector, N., Guenette, M., & Richter, M. (2020). Pregnancy and Delivery
Outcomes Following Benzodiazepine Exposure: A Systematic Review and
Meta-analysis. Canadian journal of psychiatry. Revue canadienne de psychiatrie,
65(12), 821–834. https://doi.org/10.1177/0706743720904860
Hamilton, M., (1960). A rating scale for depression. Journal of neurology, neurosurgery, and
psychiatry, 23(1), 56–62. https://doi.org/10.1136/jnnp.23.1.56
Hankin, B. L., Demers, C. H., Hennessey, E. P., Perzow, S. E. D., Curran, M. C., Gallop, R. J.,
Hoffman, M. C., & Davis, E. P. (2023). Effect of Brief Interpersonal Therapy on
Depression During Pregnancy: A Randomized Clinical Trial. JAMA psychiatry,
e230702. Advance online publication.
https://doi.org/10.1001/jamapsychiatry.2023.0702
Horan, A., Kondas, C., & Dinsell, V. (2022). Integrating Peripartum Mental Health Education
into the Psychiatry Clerkship: a Multimodal Approach. Academic psychiatry : the
journal of the American Association of Directors of Psychiatric Residency Training and
the Association for Academic Psychiatry, 46(2), 175–179.
https://doi.org/10.1007/s40596-021-01501-3
Huybrechts, K. F., Palmsten, K., Avorn, J., Cohen, L. S., Holmes, L. B., Franklin, J. M.,
Mogun, H., Levin, R., Kowal, M., Setoguchi, S., & Hernández-Díaz, S. (2014).
Antidepressant use in pregnancy and the risk of cardiac defects. The New England
journal of medicine, 370(25), 2397–2407. https://doi.org/10.1056/NEJMoa1312828
Jiang, X., Kang, Y., Li, H., Wang, D, Shan, L., & Wang, F. (2022). Efficacy of nondrug
interventions in perinatal depression: A meta-analysis. Psychiatry Research, 317.
https://doi-org/10.1016/j.psychres.2022.114916
Jordan, S., Bromley, R., Damase-Michel, C., Given, J., Komninou, S., Loane, M., Marfell, N.,
& Dolk, H. (2022). Breastfeeding, pregnancy, medicines, neurodevelopment, and
population databases: the information desert. International breastfeeding journal,
17(1), 55. https://doi.org/10.1186/s13006-022-00494-5
Kaplan, Y. C., & Demir, O. (2021). Use of Phenytoin, Phenobarbital Carbamazepine,
Levetiracetam Lamotrigine and Valproate in Pregnancy and Breastfeeding: Risk of
Major Malformations, Dose-dependency, Monotherapy vs Polytherapy,
Pharmacokinetics and Clinical Implications. Current neuropharmacology, 19(11),
1805–1824. https://doi.org/10.2174/1570159X19666210211150856
Kato, T., Kachi, Y., Ochi, M., Nagayoshi, M., Dhungel, B., Kondo, T., & Takehara, K. (2023).
The long-term association between paternal involvement in infant care and children's
psychological well-being at age 16 years: An analysis of the Japanese Longitudinal
Survey of Newborns in the 21st Century 2001 cohort. Journal of affective disorders,
324, 114–120. https://doi.org/10.1016/j.jad.2022.12.075
Kelty, E., Terplan, M., Greenland, M., & Preen, D. (2021). Pharmacotherapies for the
Treatment of Alcohol Use Disorders During Pregnancy: Time to Reconsider?. Drugs,
81(7), 739–748. https://doi.org/10.1007/s40265-021-01509-x
Khan, S. J., Fersh, M. E., Ernst, C., Klipstein, K., Albertini, E. S., & Lusskin, S. I. (2016).
Bipolar Disorder in Pregnancy and Postpartum: Principles of Management. Current
psychiatry reports, 18(2), 13. https://doi.org/10.1007/s11920-015-0658-x
Kim, M., Kang, S. K., Yee, B., Shim, S. Y., & Chung, M. (2016). Paternal involvement and
early infant neurodevelopment: the mediation role of maternal parenting stress.
BMC pediatrics, 16(1), 212. https://doi.org/10.1186/s12887-016-0747-y
Kobayashi, T., Matsuyama, T., Takeuchi, M., & Ito, S. (2016). Autism spectrum disorder and
prenatal exposure to selective serotonin reuptake inhibitors: A systematic review and
meta-analysis. Reproductive toxicology (Elmsford, N.Y.), 65, 170–178.
https://doi.org/10.1016/j.reprotox.2016.07.016
Kunkler, C., Lewis, A. J., & Almeida, R. (2022). Methamphetamine exposure during
pregnancy: A meta-analysis of child developmental outcomes. Neuroscience and
biobehavioral reviews, 138, 104714. https://doi.org/10.1016/j.neubiorev.2022.104714
Lasseter, K. Y. (2022). Antidepressants Guide. Instagram. Retrieved March 2, 2023, from
https://www.instagram.com/the.reproductive.psychiatrist/guide/antidepressants
Louw K. A. (2018). Substance use in pregnancy: The medical challenge. Obstetric medicine,
11(2), 54–66. https://doi.org/10.1177/1753495X17750299
Li, M., Francis, E., Hinkle, S. N., Ajjarapu, A. S., & Zhang, C. (2019). Preconception and
Prenatal Nutrition and Neurodevelopmental Disorders: A Systematic Review and
Meta-Analysis. Nutrients, 11(7), 1628. https://doi.org/10.3390/nu11071628
Marraccini, M. E., & Gorman, K. S. (2015). Exploring Placentophagy in Humans:
Problems and Recommendations. Journal of midwifery & women's health, 60(4),
371–379. https://doi.org/10.1111/jmwh.12309
Martin G. I. (2020). Marijuana: the effects on pregnancy, the fetus, and the newborn. Journal
of perinatology : official journal of the California Perinatal Association, 40(10),
1470–1476. https://doi.org/10.1038/s41372-020-0708-z
Massachusetts General Hospital Center for Women's Mental Health. (2020, August 18).
Lamotrigine (Lamictal) Dosing During Pregnancy. Retrieved June 14, 2023, from https://womensmentalhealth.org/posts/lamotrigine-lamictal-dosing-during-pregnancy/
Massachusetts General Hospital Center for Women's Mental Health. (2022, August 22).
Psychiatric disorders during pregnancy. Retrieved April 4, 2023, from
https://womensmentalhealth.org/specialty-clinics-2/psychiatric-disorders-during-
MDCalc. (n.d.). Hamilton depression rating scale (HAM-D).
https://www.mdcalc.com/calc/10043/hamilton-depression-rating-scale-ham-d
Meador, K. J., Baker, G. A., Browning, N., Cohen, M. J., Bromley, R. L., Clayton-Smith, J.,
Kalayjian, L. A., Kanner, A., Liporace, J. D., Pennell, P. B., Privitera, M., Loring, D. W.,
& Neurodevelopmental Effects of Antiepileptic Drugs (NEAD) Study Group (2014).
Breastfeeding in children of women taking antiepileptic drugs: cognitive outcomes at
age 6 years. JAMA pediatrics, 168(8), 729–736.
https://doi.org/10.1001/jamapediatrics.2014.118
Mehta, T. M., & Van Lieshout, R. J. (2017). A review of the safety of clozapine during
pregnancy and lactation. Archives of women's mental health, 20(1), 1–9.
https://doi.org/10.1007/s00737-016-0670-0
Mocking, R. J. T., Steijn, K., Roos, C., Assies, J., Bergink, V., Ruhé, H. G., & Schene, A. H.
(2020). Omega-3 Fatty Acid Supplementation for Perinatal Depression: A
Meta-Analysis. The Journal of clinical psychiatry, 81(5), 19r13106.
https://doi.org/10.4088/JCP.19r13106
Monteiro, S., Nejad, Y. S., & Aucoin, M. (2022). Perinatal diet and offspring anxiety: A
scoping review. Translational neuroscience, 13(1), 275–290.
https://doi.org/10.1515/tnsci-2022-0242
Moon, R. Y., Carlin, R. F., Hand, I., & TASK FORCE ON SUDDEN INFANT DEATH
SYNDROME AND THE COMMITTEE ON FETUS AND NEWBORN (2022).
Sleep-Related Infant Deaths: Updated 2022 Recommendations for Reducing Infant
Deaths in the Sleep Environment. Pediatrics, 150(1), e2022057990.
https://doi.org/10.1542/peds.2022-057990
Muzik, M., & Hamilton, S. E. (2016). Use of Antidepressants During Pregnancy?: What to
Consider when Weighing Treatment with Antidepressants Against Untreated
Depression. Maternal and child health journal, 20(11), 2268–2279.
https://doi.org/10.1007/s10995-016-2038-5
Muzik, M., Hamilton, S. E., Lisa Rosenblum, K., Waxler, E., & Hadi, Z. (2012). Mindfulness
yoga during pregnancy for psychiatrically at-risk women: preliminary results from
a pilot feasibility study. Complementary therapies in clinical practice, 18(4),
235–240. https://doi.org/10.1016/j.ctcp.2012.06.006
Nagpal, T. S., Bhattacharjee, J., da Silva, D. F., Souza, S. C. S., Mohammad, S., Puranda, J.
L., Abu-Dieh, A., Cook, J., & Adamo, K. B. (2020). Physical activity may be an
adjuvant treatment option for substance use disorders during pregnancy: A
scoping review. Birth defects research, 113(3), 265–275.
https://doi.org/10.1002/bdr2.1803
National Center for Biotechnology Information (2023a). PubChem Compound Summary for
CID 23663956, Divalproex sodium. Retrieved June 21, 2023 from
https://pubchem.ncbi.nlm.nih.gov/compound/Divalproex-sodium
National Center for Biotechnology Information (2023b). PubChem Compound Summary for
CID 3549980, Valproate. Retrieved June 21, 2023 from
https://pubchem.ncbi.nlm.nih.gov/compound/Valproate.
Noh, Y., Lee, H., Choi, A., Kwon, J. S., Choe, S. A., Chae, J., Kim, D. S., & Shin, J. Y. (2022).
First-trimester exposure to benzodiazepines and risk of congenital malformations in
offspring: A population-based cohort study in South Korea. PLoS medicine, 19(3),
e1003945. https://doi.org/10.1371/journal.pmed.1003945
Nulman, I., Rovet, J., Stewart, D. E., Wolpin, J., Gardner, H. A., Theis, J. G., Kulin, N., &
Koren, G. (1997). Neurodevelopment of children exposed in utero to
antidepressant drugs. The New England journal of medicine, 336(4), 258–262.
https://doi.org/10.1056/NEJM199701233360404
Payne J. L. (2021). Psychiatric Medication Use in Pregnancy and Breastfeeding.
Obstetrics and gynecology clinics of North America, 48(1), 131–149.
https://doi.org/10.1016/j.ogc.2020.11.006
Poyatos-León, R., García-Hermoso, A., Sanabria-Martínez, G., Álvarez-Bueno, C.,
Cavero-Redondo, I., & Martínez-Vizcaíno, V. (2017). Effects of exercise-based
interventions on postpartum depression: A meta-analysis of randomized
controlled trials. Birth (Berkeley, Calif.), 44(3), 200–208.
https://doi.org/10.1111/birt.12294
Prince, M. K., Daley, S. F., & Ayers, D. (2023). Substance Use in Pregnancy. In StatPearls.
StatPearls Publishing.
Ramadan, E. F., Grisdale, M., & Morais, M. (2022). Maternal Vitamin B12 Levels During
Pregnancy and Their Effects on Maternal Neurocognitive Symptoms: A
Systematic Review. Journal of obstetrics and gynaecology Canada : JOGC =
Journal d'obstétrique et gynécologie du Canada : JOGC, 44(4), 390–394.e3.
https://doi.org/10.1016/j.jogc.2021.11.017
Rogers, A., Obst, S., Teague, S. J., Rossen, L., Spry, E. A., Macdonald, J. A., Sunderland,
M., Olsson, C. A., Youssef, G., & Hutchinson, D. (2020). Association Between
Maternal Perinatal Depression and Anxiety and Child and Adolescent
Development: A Meta-analysis. JAMA pediatrics, 174(11), 1082–1092.
https://doi.org/10.1001/jamapediatrics.2020.2910
Sankaran, D., Lakshminrusimha, S., & Manja, V. (2022). Methamphetamine: burden,
mechanism and impact on pregnancy, the fetus, and newborn. Journal of perinatology:
official journal of the California Perinatal Association, 42(3), 293–299.
https://doi.org/10.1038/s41372-021-01271-8
Sheffield, K. M., & Woods-Giscombé, C. L. (2016). Efficacy, Feasibility, and Acceptability of
Perinatal Yoga on Women's Mental Health and Well-Being: A Systematic Literature
Review. Journal of holistic nursing : official journal of the American Holistic Nurses'
Association, 34(1), 64–79. https://doi.org/10.1177/0898010115577976
Skilbeck, L., Spanton, C., & Roylance, I. (2023). Recognition and CBT for Paternal
Perinatal Depression in Primary Care: A Case Report. American journal of men's
health, 17(2), 15579883231159955.
https://doi.org/10.1177/15579883231159955
Szpunar, M. J., Freeman, M. P., Kobylski, L. A., Caplin, P. S., Gaccione, P., Viguera, A. C.,
Chitayat, D., Hernández-Díaz, S., & Cohen, L. S. (2022). Risk of major malformations
in infants after first-trimester exposure to benzodiazepines: Results from the
Massachusetts General Hospital National Pregnancy Registry for Psychiatric
Medications. Depression and anxiety, 39(12), 751–759.
https://doi.org/10.1002/da.23280
Ssewanyana, D., Knight, J. A., Matthews, S. G., Wong, J., Khani, N. A., Lye, J., Murphy, K. E.,
Foshay, K., Okeke, J., Lye, S. J., & Hung, R. J. (2022). Maternal prenatal
psychological distress and vitamin intake with children's neurocognitive development.
Pediatric research, 92(5), 1450–1457. https://doi.org/10.1038/s41390-022-02003-0
Standeven, L. R., Osborne, L. M., Betz, J. F., Yenokyan, G., Voegtline, K., Hantsoo, L., &
Payne, J. L. (2022). Allopregnanolone and depression and anxiety symptoms
across the peripartum: an exploratory study. Archives of women's mental health,
25(2), 521–526. https://doi.org/10.1007/s00737-021-01186-5
Tirani, S. A., Balali, A., Askari, G., & Saneei, P. (2023). Maternal serum 25-hydroxy vitamin
D levels and risk of autism spectrum and attention-deficit hyperactivity disorders
in offspring: A systematic review and dose-response meta-analysis. Psychiatry
research, 319, 114977. https://doi.org/10.1016/j.psychres.2022.114977
Uguz F. (2016). Second-Generation Antipsychotics During the Lactation Period: A
Comparative Systematic Review on Infant Safety. Journal of clinical
psychopharmacology, 36(3), 244–252.
https://doi.org/10.1097/JCP.0000000000000491
Upadhyaya, S., Ståhlberg, T., Silwal, S., Arrhenius, B., & Sourander, A. (2022). Maternal
Vitamin D Levels during Pregnancy and Offspring Psychiatric Outcomes: A
Systematic Review. International journal of molecular sciences, 24(1), 63.
https://doi.org/10.3390/ijms24010063
Ventriglio, A., Sancassiani, F., Contu, M. P., Latorre, M., Di Slavatore, M., Fornaro, M.,
& Bhugra, D. (2020). Mediterranean Diet and its Benefits on Health and
Mental Health: A Literature Review. Clinical practice and epidemiology in
mental health : CP & EMH, 16(Suppl-1), 156–164.
https://doi.org/10.2174/1745017902016010156
Viguera, A. C., Freeman, M. P., Kobylski, L. A., Rossa, E. T., Gaccione, P., Chitayat, D.,
Hernández-Díaz, S., & Cohen, L. S. (2023). Risk of Major Malformations Following
First-Trimester Exposure to Olanzapine: Preliminary Data From the Massachusetts
General Hospital National Pregnancy Registry for Psychiatric Medications. Journal of
clinical psychopharmacology, 43(2), 106–112.
https://doi.org/10.1097/JCP.0000000000001665
Viswanathan, M., Middleton, J. C., Stuebe, A. M., Berkman, N. D., Goulding, A. N.,
McLaurin-Jiang, S., Dotson, A. B., Coker-Schwimmer, M., Baker, C., Voisin, C. E.,
Bann, C., & Gaynes, B. N. (2021). Maternal, Fetal, and Child Outcomes of Mental Health Treatments in Women: A Meta-Analysis of Pharmacotherapy. Psychiatric research and clinical practice, 3(3), 123–140. https://doi.org/10.1176/appi.prcp.20210001
Wall-Wieler, E., Robakis, T. K., Lyell, D. J., Masarwa, R., Platt, R. W., & Carmichael, S. L.
(2020). Benzodiazepine use before conception and risk of ectopic pregnancy.
Human reproduction (Oxford, England), 35(7), 1685–1692.
https://doi.org/10.1093/humrep/deaa082
Wang, D., Li, Y. L., Qiu, D., & Xiao, S. Y. (2021). Factors Influencing Paternal Postpartum
Depression: A Systematic Review and Meta-Analysis. Journal of affective
disorders, 293, 51–63. https://doi.org/10.1016/j.jad.2021.05.088
Wang, X., Zhang, T., Ekheden, I., Chang, Z., Hellner, C., Jan Hasselström,
Jayaram-Lindström, N., M D'Onofrio, B., Larsson, H., Mataix-Cols, D., & Sidorchuk, A.
(2022). Prenatal exposure to benzodiazepines and Z-drugs in humans and risk of
adverse neurodevelopmental outcomes in offspring: A systematic review.
Neuroscience and biobehavioral reviews, 137, 104647.
https://doi.org/10.1016/j.neubiorev.2022.104647
Zepeda, R. C., Juárez-Portilla, C., & Molina-Jiménez, T. (2023). St. John's Wort usage in
treating of perinatal depression. Frontiers in behavioral neuroscience, 16,