Episode 119: Obsessive Compulsive Disorder (OCD)
By listening to this episode, you can earn 1.25 Psychiatry CME Credits.
Other Places to listen: iTunes, Spotify
Article Authors: Chantel Fletcher, Amanda Shim, Dr. Ariana Martinez, Dr. Joseph Wong, Dr. Michael Cummings, Dr. David Puder
There are no conflicts of interest to report for this episode.
Introduction
Obsessive-compulsive disorder (OCD) is a condition characterized by the presence of obsessions and compulsions, which can manifest in multiple ways. Obsessions are recurrent, intrusive thoughts that provoke anxiety. The distress from these obsessions often leads to the development of compulsions. These are repetitive behaviors or mental actions performed to provide temporary relief (Penzel, 2000).
This results in a vicious cycle: obsession → anxiety → compulsion → reinforcement → repeat. Patients are aware (to varying degrees) of the irrationality of their thoughts and behaviors. However, this is not enough to break the cycle. (Heyman, 2006).
OCD extends beyond traits of being particular, meticulous, or occasionally displaying obsessive or compulsive tendencies (Penzel, 2000). It is important to distinguish between what is pathological vs. normal. With this disorder, the frequency and intensity of thoughts and preoccupations impair socio-occupational functioning (Fornaro, 2009).
It is also necessary to differentiate between compulsivity and impulsivity. A compulsive individual is doubtful, over-controlled, risk-averse, and acts with fear of consequences. An impulsive individual is mildly doubtful (if at all), under-controlled, stimulation-seeking, and acts with little to no thought of consequences. With OCD, compulsions are not performed for pleasure, although individuals usually experience relief from anxiety or distress (Penzel, 2000).
Obsessive thoughts are multifactorial. They can be abrupt or gradual, convincing or ridiculous, same or different, and persistent or intermittent. Regardless, obsessions are centered around consistent themes (Penzel, 2000). In a case study by Richter et al., a 35-year-old man described concerns of contamination that began as a teenager but had become problematic over the last few years. These were accompanied by a fear of accidentally infecting and harming his family with germs. As a result, this individual washed his hands at least twenty times a day using soap or hand sanitizer. In addition, he would spend several hours cleaning and taking showers. However, over the last two years, these compulsions grew increasingly intense and time-consuming. He began to avoid both direct and indirect contact, from shaking hands to sharing pens. In addition, he limited visits with his parents out of fear of making them ill (Richter, 2018).
Another classic feature that accompanies this disorder is the sense or feeling of uncertainty despite assurance and information. These individuals simultaneously believe and do not believe in their obsessions. Even though there is no real cause-effect relationship, this doubt makes it difficult for them to function normally (Penzel, 2000).
Treatment of OCD, which will be explored more fully later, typically involves multiple modalities, including pharmaceutical (e.g., SSRIs, SNRIs, TCAs) and psychotherapeutic (e.g., cognitive behavioral therapy). It is essential to recognize the signs and symptoms of this disorder as patients may be unaware or unwilling to share this information. For example, they may hide their obsessions and compulsions or build them into the infrastructure of daily life.
Neurobiology of OCD
Based on neuroimaging studies, the cortico-striatal-thalamic-cortical loop (CSTC) is thought to be the critical brain circuit involved in the pathophysiology of OCD. Specifically, research suggests hyperactivity of the orbitofrontal cortex, anterior cingulate cortex, and striatum. Dysfunction may lead to implicit processing deficits and intrusive symptoms in patients with OCD (Parmar, 2016).
In addition, studies found that OCD patients abnormally utilized the hippocampus with implicit sequence-learning tasks, while healthy subjects utilized the striatum during the performance of cognitive tasks (Simpson, 2020b).
A meta-analysis comparing 412 OCD patients with 368 healthy subjects found abnormalities in the dorsomedial prefrontal cortex, inferior frontal gyrus, and cerebellum (Simpson, 2020b).
Although abnormalities in serotonergic and dopamine signaling in cortico-striatal pathways are hypothesized to contribute to the pathophysiology of OCD, pharmacological challenge studies have been inconclusive. Of note, defects in glutamatergic signaling have also been examined. However, magnetic resonance spectroscopy studies have been inconclusive (Simpson, 2020b).
Brennan et al. reviewed 28 studies regarding the quantification of neurochemicals in the CSTC loop for patients with OCD. Despite mixed results, this study identified particular areas warranting further research, including the 1) reduced tNAA in the ACC and caudate, 2) reduced Glx in the ACC, 3) increased Glx in the caudate, and 4) increased tCho in the thalamus, parietal white matter, and hippocampus (Brennan, 2013).
OCD in History and Literature
Obsessive-compulsive disorder is not a new phenomenon, and descriptions of signs and symptoms can be found in historical documents over several centuries.
A 15th-century anthology regarding witchcraft and psychopathology entitled Malleus Maleficarum (The Witch’s Hammer) describes compulsions displayed by a priest thought to be possessed by the devil (Fornaro, 2009):
“[W]hen he passed any church, and genuflected in honour of the Glorious virgin, the devil made him thrust his tongue far out of his mouth when he tried to engage in prayer; [the devil] attacked him more violently.”
In the 17th-century Shakespearean play Macbeth, Lady McBeth exhibited compulsive hand-washing following the assassination of King Duncan (Fornaro, 2009):
“It is an accustomed action with her, to seem thus washing her hands. I have known her continue in this a quarter of an hour.”
Over time, the explanation for obsessions and compulsions shifted from religious to medical models. In 1838, descriptions of this disorder were published by French psychiatrist Jean-Étienne Dominique Esquirol. German psychiatrist Carl Westphal identified differences between obsessions and compulsions in 1877 (Oberbeck, 2013). By the end of the 19th century, obsessions and compulsions were understood to be manifestations of melancholy and depression (Fornaro, 2009). Our understanding of these symptoms underwent a further change, as evidenced by Pierre Janet and Sigmund Freud. Janet's work, Obsessions and Psychasthenia (1903) outlined treatment of "forceful agitations," while Freud's case study, Notes upon a Case of Obsessional Neurosis (1909), focused on psychoanalysis (Pittman, 1987; Fornaro, 2009).
In the 1950s, as behavioral therapy gained precedence, the learning theories that helped conceptualize and treat phobic disorders were applied to OCD. Though they failed to address all symptoms of OCD, these efforts led to the development of more effective ways to reduce compulsions in the 1960s and 1970s. During the 1980s, research concentrated on the relationship between this disorder and neurological issues (e.g., epilepsy, memory disorders, Tourette's syndrome) (Fornaro, 2009).
Since the 1990s, OCD and obsessive-compulsive and related disorders (OCRDs) have been grouped with a broad spectrum of related disorders due to overlapping clinical manifestations (Fornaro, 2009). The DSM-5 now considers OCD among OCRDs in contrast to its classification as an anxiety disorder in previous editions (Stein, 2010).
Epidemiology
Who is Affected?
For OCD, lifetime prevalence is approximately 2.5% (Richter, 2018). In the United States, prevalence is 2.3% for adults, with the ratio of affected males to females approximately 1:1 (Ruscio, 2010; Grant, 2014). For children, prevalence is 1-2% (Geller, 2012). However, unlike adult-onset OCD, the manifestation of this disorder in younger age groups differs between males and females. With childhood-onset OCD, the males are more affected than females with a ratio of 2:1-3:1. Conversely, with adolescent-onset OCD, females are more affected than males with a ratio of 1:1.4 (Grant, 2014).
Age of onset typically follows a bimodal pattern with the first peak at 10 years (occurring in childhood) and the second peak at 19-21 years (occurring during adolescence or young adulthood) (Grant, 2014). The mean age of onset for all age groups is 19.5 years (Ruscio, 2010). Of note, emergence after the age of 30 is atypical (Grant, 2014).
Risk Factors
Genetic Factors:
The rate of onset among first-degree relatives of adults with the disorder is two times higher than first-degree relatives of adults without the disorder. Nevertheless, the rate is 10x higher among first-degree relatives of individuals with childhood or adolescent-onset OCD (American Psychiatric Association, 2013).
There is a reported 45%-65% heritability for childhood-onset OCD and 27%-47% for adolescent or adult-onset OCD (van Grootheest, 2005).
For reference:
Height:
Heritability: 89-93% (Silventoinen, 2003)
ADHD:
Heritability: 71-73% (Nikolas, 2010)
Schizophrenia:
Heritability: 73% (Hilker, 2018)
Bipolar:
Heritability: 60% (Johansson, 2019)
BPD:
Heritability: 46% (Skoglund, 2021)
The concordance rate is reported to be 0.57 for monozygotic twins and 0.22 for dizygotic twins (Pauls, 2010).
Developmental and Psychosocial and Factors:
There are various developmental factors beginning in childhood associated with adult-onset OCD. These include abuse, neglect, isolation, and bullying (Veale, 2014). Negative emotionality and internalizing symptoms are also risk factors (Grisham, 2011).
In addition, stressful life events (e.g., parents getting divorced, breaking up with a significant other, failing exams) are associated with adolescent-onset OCD (Krebs, 2019).
Gender-Related Differences
Compared to females, males have an earlier age at onset and a higher likelihood of a comorbid tic disorder with OCD (American Psychiatric Association, 2013).
There have been reported gender differences in the manifestation of symptoms. Males are more likely to have symptoms regarding symmetry or forbidden thoughts, while females are more likely to have symptoms regarding cleaning (American Psychiatric Association, 2013).
Emerging or worsening OCD has been observed in the peripartum period leading to disruption of the mother-infant relationship. For example, if the mother is experiencing aggressive obsessions, this may lead to avoidance of the infant (American Psychiatric Association, 2013).
Suicide Risk
For OCD, suicidal ideation can present in up to half, and actual attempts are evident in up to one-quarter of individuals. The accompaniment of major depressive disorder increases this risk (American Psychiatric Association, 2013).
Assessment and Clinical Manifestations
DSM-5 (American Psychiatric Association, 2013)
DSM-5 Diagnostic Criteria 300.3 (F42.2 F42) and link to table format
Presence of obsessions, compulsions, or both
Obsessions are defined by (1) and (2):
Recurrent and persistent thoughts, urges, or images that are experienced at some time during the disturbance as intrusive and unwanted and that in most individuals cause marked anxiety or distress.
The individual attempts to ignore or suppress such thoughts, urges, or images, or to neutralize them with some other thought or action (i.e., by performing a compulsion).
Compulsions are defined by (1) and (2):
Repetitive behaviors (e.g., hand washing, ordering, checking) or mental acts (e.g., praying, counting, repeating words silently) that the individual feels driven to perform in response to an obsession or according to rules that must be applied rigidly.
The behaviors or mental acts are aimed at preventing or reducing anxiety or distress, or preventing some dreaded event or situation; however, these behaviors or mental acts are not connected in a realistic way with what they are designed to neutralize or prevent, or are clearly excessive.
Note: Young children may not be able to articulate the aims of these behaviors or mental acts.
The obsessions or compulsions are time-consuming (e.g., take more than 1 hour per day) or cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The obsessive-compulsive symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition.
The disturbance is not better explained by the symptoms of another mental disorder (e.g., excessive worries, as in generalized anxiety disorder; preoccupation with appearance, as in body dysmorphic disorder; difficulty discarding or parting with possessions, as in hoarding disorder; hair pulling, as in trichotillomania [hair-pulling disorder]; skin picking, as in excoriation [skin-picking] disorder; stereotypies, as in stereotypic movement disorder; ritualized eating behavior, as in eating disorders; preoccupation with substances or gambling, as in substance-related and addictive disorders; preoccupation with having an illness, as in illness anxiety disorder; sexual urges or fantasies, as in paraphilic disorders; impulses, as in disruptive, impulse-control, and conduct disorders; guilty ruminations, as in major depressive disorder; thought insertion or delusional preoccupations, as in schizophrenia spectrum and other psychotic disorders; or repetitive patterns of behavior, as in autism spectrum disorder).
Specify if:
With good or fair insight: The individual recognizes that obsessive-compulsive disorder beliefs are definitely or probably not true or that they may or may not be true.
With poor insight: The individual thinks obsessive-compulsive disorder beliefs are probably true.
With absent insight/delusional beliefs: The individual is completely convinced that obsessive-compulsive disorder beliefs are true.
Specify if:
Tic-related: The individual has a current or past history of a tic disorder.
Yale-Brown Obsessive Compulsive Scale (Y-BOCS)
Y-BOCS link to scale and symptom checklist PDF
The Y-BOCS is the most widely used standardized rating scale for OCD. It consists of a checklist and scale designed to rate symptom severity and to establish a diagnosis. In addition, clinicians can assess new patients and monitor the course of disorder and response to treatment. There are two versions available, observer-rated and self-report (Goodman, 1989). As some of these questions may be considered distressing to talk about, it may be beneficial to develop a therapeutic alliance before utilizing the Y-BOCS.
Scoring: There are ten items covering five dimensions for obsession and compulsions: Time spent or occupied; interference with functioning or relationships; degree of distress; resistance; and control (Goodman, 1989):
Each item is scored on a 4 point scale from 0 (no symptoms) to 4 (extreme symptoms) with a total range from 0-40. In addition, there are separate subtotals depending on the severity of obsessions and compulsions. A score of less than 7 is considered subclinical; 8-15 mild; 16-23 moderate; 24-31 severe; 32-40 extreme.
Overall, the Y-BOCS demonstrates good convergent validity compared to other measures of OCD. The internal consistency is acceptable but can be improved by excluding items involving resistance to obsessions and compulsions as in the revised 9-item Y-BOCS (Woody, 1995). When comparing the observed-rated vs. self-report versions, findings suggest that the latter may be preferable for clinicians when considering time and money due to internal consistency and test-retest reliability. The only consideration to be aware of is that patients tend to report more symptoms on the self-report (Steketee, 1996).
Children’s Yale-Brown Obsessive Compulsive Scales (CY-BOCS): The CY-BOCS is a modified version of the Y-BOCS. It has a similar structure, points, and scoring but with different wording of questions to be more appropriate for children and adolescents (Scahill, 1997). CY-BOCS link to scale and symptom checklist PDF.
Clinical Applicability: Clinical presentations are diverse, and obsessions and compulsions are not restricted to the examples in the Y-BOCS. Regardless of the manifestation of symptoms, the only requirement is to fit the obsession-compulsion relationship. Though obsessions can virtually cover any topic, it is possible to organize them into categories or themes. This aids the process of identifying triggers as well as compulsions. Examples are provided in the Y-BOCS and CY-BOCS (Hershfield, 2013).
Subtypes: According to Hershfield, two subtypes that differ in presentation from others are “just right” OCD (also referred to as symmetry OCD, organizational OCD, or perfectionism OCD) and hyperawareness OCD (Hershfield, 2013).
“Just Right” OCD: There are elements of perfectionism present in many facets of OCD. However, “just right” OCD is different in that perfectionism is the method to avoid negative consequences. This subtype is characterized by feelings of incompleteness and that something is not “right.” When these feelings are not addressed, there can be superimposed anxiety. There is usually no specific consequence of imperfection that individuals can distinctly express (Penzel, 2000; Hershfield, 2013):
Examples of “just right” obsessions: Fear of not knowing everything about a topic, questioning whether something was said or done perfectly.
Examples of “just right” compulsions: Repeatedly checking known information, only performing certain activities at perfect times.
Hyperawareness OCD: As the name suggests, hyperawareness OCD involves being consciously and excessively aware of something innocuous, more so than others. It can include somatic obsessions and many other miscellaneous obsessions (Penzel, 2000; Hershfield, 2013):
Examples of somatic obsessions: Excessive awareness of involuntary bodily processes of known or unknown origin (e.g., body position, breathing, heartbeat).
Examples of other miscellaneous obsessions: Excessive awareness of their own thought processes, people’s subtle physical movements, or size or location of particular objects.
Examples of hyperawareness compulsions: Mental checking for the trigger, conscious examination of the nature or significance of the trigger, reassurance or avoidance of the trigger.
Course of the Disorder
Without treatment, the course of the disorder is often chronic with waxing and waning symptoms. Some individuals can have an intermittent course, while a minority can have a deteriorating course. Adult remission rates are low (e.g., 20% of individuals re-evaluated in 40 years). Onset in childhood or adolescence can lead to lifelong OCD, but 40% of these individuals may experience a decline in symptoms by early adulthood (American Psychiatric Association, 2013).
Functional Consequences
OCD can lead to lower quality of life and higher levels of social and occupational impairment. Impairment extends into daily life and depends on symptom severity. It can be attributed to (Simpson, 2020b):
Time lost due to focusing on obsessions and acting on compulsions.
Avoidance of triggering situations.
Specific symptoms can create obstacles, including:
Obsessions about harm may disrupt dynamics with family and friends because they make the relationships feel dangerous.
Obsessions about symmetry may impede the completion of time-sensitive projects, such as those at work or school because they do not feel “just right.”
Obsessions about contamination may lead to the avoidance of healthcare professionals due to fears of germs or development of skin issues due to excessive washing.
Lastly, sometimes this disorder interferes with its own treatment (e.g., fear of medication being contaminated or unsafe in some way).
Early onset of this disorder may lead to developmental difficulties. For example, children or adolescents may refrain from socializing with family, friends, or colleagues. In addition, they may also have difficulty leaving home and living independently (Simpson, 2020b).
Individuals with OCD may attempt to impose rules on their family, leading to accommodation and participation in their obsessions and compulsions. Family members may help to avoid triggers or take part in compulsions. For example, they may forbid their families from inviting visitors due to fears of contamination. This can contribute to a high burden and reduced quality of life among family members (Simpson, 2020b).
Differential Diagnosis
OCD vs. Obsessive-Compulsive Personality Disorder (OCPD)
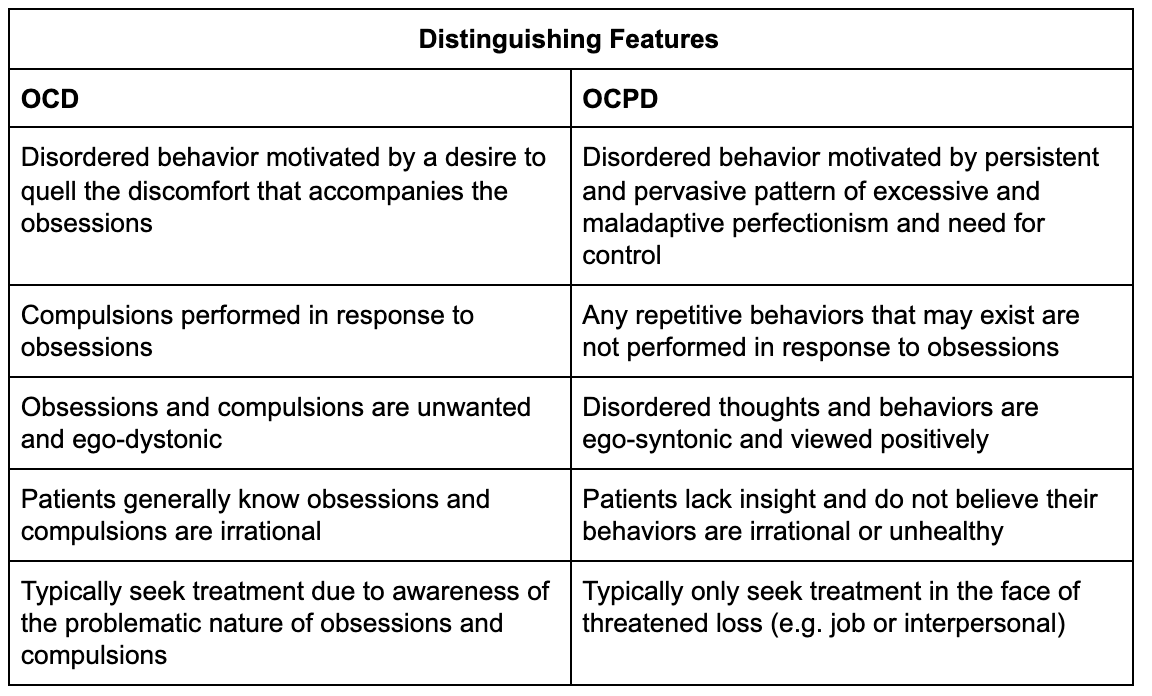
Despite having similar names, these two disorders present with different clinical manifestations. OCPD is characterized by a persistent and pervasive pattern of perfectionism and control (American Psychiatric Association, 2013). Individuals have a sense of righteousness about how things “should be done” and an unwillingness to give responsibilities to others. They display rigid adherence to rules and regulations within their comfort zones. With OCPD, repetitive behaviors are not performed in relation to obsessions (American Psychiatric Association, 2013). Individuals with this disorder have ego-syntonic symptoms, meaning their thoughts and tendencies align with how they view themselves, but they do not think anything is wrong. (Skodol, 2018). As a result, they will most likely only be motivated to seek treatment from the threat of losing a job or an interpersonal relationship (Penzel, 2000). With OCD, patients typically recognize that their unwanted thoughts are unreasonable and find them unpleasant. In this way, they experience ego-dystonic symptoms and see these obsessions and compulsions at odds with their self-concept (Rosenberg, 2019). If an individual manifests symptoms of both disorders, a dual diagnosis may be given (American Psychiatric Association, 2013).
OCD vs. Trichotillomania (TTM)
TTM is characterized by constant hair pulling from various sites leading to observable hair loss. TTM and OCD are similar in the sense of being unable to avoid performing a particular behavior. However, unlike OCD, the act of hair pulling is not in response to obsessive thoughts but rather the promise of gratification with TTM. In other words, OCD is considered ego-dystonic, while TTM is considered ego-syntonic. Symptoms of OCD may also change in focus and severity while symptoms of TTM stay the same without evolution to other rituals (Lochner, 2005).
OCD vs. Body Dysmorphic Disorder (BDD)
BDD is defined as a preoccupation with one or more flaws in physical appearance that is imagined or not noticeable to others. Excessive repetitive behaviors or mental acts are performed in response to these perceived defects, including mirror checking, excessive grooming, hiding blemished areas, or comparing with other people. While OCD virtually covers any topic, BDD is strictly about appearance. In addition, individuals with BDD may have poorer insight on average than those with OCD. It is possible to have both OCD and BDD (American Psychiatric Association, 2013).
OCD vs. Hoarding Disorder
Hoarding disorder is characterized by extreme difficulty and significant distress separating with or discarding of personal belongings (American Psychiatric Association, 2013). The primary motivators are emotional attachment, potential usefulness, aesthetic value of the objects, and avoidance of wastefulness. In the DSM-IV, characteristics indicative of hoarding disorder were previously assigned to OCD and OCPD. However, the DSM-5 now designates it as a standalone diagnosis (Mataix-Cols, 2014). Although individuals with the previously mentioned disorders can exhibit behaviors associated with hoarding disorder, full diagnostic criteria must be met for diagnosis. With OCD, these behaviors are usually the result of specific obsessions. They are not associated with genuine desire and provoke significant distress. Of note, the items collected by these individuals tend to be minimal but bizarre. Conversely, individuals with hoarding disorder may have considerably less insight compared to those with OCD. It is also possible for these disorders to co-exist (American Psychiatric Association, 2013).
OCD vs. Tics (Tic Disorder) and Stereotyped Movements
A tic is a sudden, quick, repetitive, nonrhythmic movement or vocalization, while a stereotyped movement is a recurrent, seemingly driven, nonfunctional motor activity. Compared to OCD, these are not performed in response to obsessions and are usually less complex than compulsions. Regardless, it is sometimes difficult distinguishing between tics and compulsions. While obsessions precede compulsions, tics are preceded by premonitory sensory urges. Individuals can have both of these disorders warranting two diagnoses (American Psychiatric Association, 2013).
OCD vs. Anxiety Disorders
Individuals with anxiety disorders also display recurrent thoughts, avoidant behaviors, and requests for reassurance (American Psychiatric Association, 2013):
With GAD, these fears stem from real-life concerns as opposed to questionable obsessions with OCD. In addition, there is a lack of compulsions with GAD.
Similar to OCD, specific phobias involve fear of specific objects or situations. However, these are more delimited and lack rituals.
Regarding SAD (also referred to as social phobia), fears and attempts of avoidance or reassurance are restricted to social interactions.
OCD vs. Eating Disorders
Anorexia nervosa is restricted to concerns about food and weight in contrast to the broad spectrum of themes covered by OCD. Individuals with anorexia nervosa also demonstrate prominent behaviors, including distorted self-image, fear of weight gain, and restrictive intake (American Psychiatric Association, 2013). Table
OCD vs. Schizophrenia
It is essential to distinguish the illogical or superstitious nature of obsessions from the delusions and hallucinations of schizophrenia (Penzel, 2000). With OCD, patients may have poor insight or delusional beliefs. However, the presence of obsessions and compulsions distinguish them from delusional disorder. In addition, these individuals lack features of schizophrenia or schizoaffective disorder such as hallucinations or formal thought disorder (American Psychiatric Association, 2013). In addition, patients with OCD recognize that their obsessions are generated within their own minds, whereas patients with schizophrenia believe their thoughts are being broadcast from external sources. OCD is characterized by doubtfulness, and patients understand that their obsessions may seem crazy. On the other hand, patients with schizophrenia stand by their delusions and hallucinations with little or no doubt in their minds (Penzel, 2000). Their touch with reality, capacity to reason, and insight are impaired. An individual can have both schizophrenia and OCD (American Psychiatric Association, 2013).
Investigators have reported prevalence rates of OCS in the schizophrenia population of 10%–52% and of OCD in the schizophrenia population of 7.8%–26% (Bottas, 2005). Studies suggest this is due to treatment with atypical antipsychotics, particularly clozapine. There was a higher rate of OCS and OCD in schizophrenic patients treated with atypical antipsychotics than the general population of approximately 26.6% vs. 1–3%. This is suspected due to decreased D2-blocking, increased 5-HT2A and 5-HT2C blocking effects, and stronger glutamate-transmission enhancing properties. As a result, such cases require careful diagnosis and management (Grassi, 2014).
Of note, evidence suggests that patients with comorbid schizophrenia and OCD may represent a unique category among patients with schizophrenia (termed schizo-obsessive). Neurobiological data on each disorder proposes the involvement of common brain regions (e.g., basal ganglia, thalamus, anterior cingulum, orbitofrontal cortex, and regions of the temporal cortex) and neurotransmitter systems (e.g., serotonin and dopamine). In addition, neuropsychological testing has revealed more severe impairment than among patients who only have schizophrenia or OCD, implying an interaction between these disease processes. More research is needed to clarify the nature of this putative entity (Bottas, 2005).
OCD vs. Major Depressive Disorder
OCD can be differentiated from the rumination that accompanies major depressive disorder, in which thoughts are usually congruent with mood and not necessarily intrusive or distressing (American Psychiatric Association, 2013). In addition, there is no long-term history of obsessing, and ruminations are not linked to compulsions (Penzel, 2000; American Psychiatric Association, 2013). Overall, they are less doubtful and more negative global perception about life, including relationships, careers, and finances (Penzel, 2000).
OCD vs. Other Compulsive-Like Behaviors
Certain behaviors are sometimes described as “compulsive,” including gambling, substance use, and sexual behavior. However, these are different from the compulsions of OCD. For example, individuals usually derive pleasure from the activity and avoid this behavior due to potential consequences (American Psychiatric Association, 2013).
Comorbidities
Individuals with OCD are often diagnosed with other psychopathology. At some point in their lifetime, 76% of adults with this disorder may also have an anxiety disorder, while 63% may have a depressive or bipolar disorder. OCD usually develops after anxiety disorders (except separation anxiety disorder) and post-traumatic stress disorder (PTSD). Conversely, it develops before depressive disorders. In addition, OCPD may also be present in individuals with OCD (American Psychiatric Association, 2013).
Up to 30% of individuals with OCD meet the criteria for a tic disorder in their lifetime (especially males with childhood-onset OCD). Compared to those without tic disorders, they differ in symptoms, course, comorbidity, and transmission of OCD. Of note, children can have a triad of these two disorders with attention deficit hyperactivity disorder (ADHD) (American Psychiatric Association, 2013).
According to the DSM-5, there is a higher prevalence of obsessive-compulsive and related disorders, including body dysmorphic disorder, trichotillomania, and excoriation in individuals with OCD. There also seems to be a link with impulsive disorders such as oppositional defiant disorder. Of importance, 12% of individuals with schizophrenia or schizoaffective disorder meet diagnostic criteria for OCD. There are also increased rates of bipolar disorder, eating disorder, and Tourette’s disorder. As a result, individuals diagnosed with any of these disorders should also be assessed for OCD (American Psychiatric Association, 2013).
Management
Psychopharmacological Interventions
General Discussion
Although psychotherapy is the front-line treatment for OCD, medication is a helpful, and at times essential, component of management and recovery (Simpson, 2020a).
With most medications for this disorder, clinical trials are short-term. However, extended trials of clomipramine and selective serotonin reuptake inhibitors (SSRIs), which randomly assigned patients to continued medication or placebo, have shown a lower relapse rate for patients on continued medication than patients on placebo. Relapse rates are variable, partially due to differences in methodology among studies. As a result, the American Psychiatric Association (APA) practice guidelines advise that patients who are responsive to serotonergic medication continue for at least one or two years. However, this recommendation warrants further research. If the course is discontinued, the practice guidelines recommend a gradual taper (Simpson, 2020a).
Individuals with OCD are often treated with high doses of SSRIs compared to other disorders per the practice guidelines. A meta-analysis by Bloch et al. confirmed the efficacy of high doses compared to low or medium doses of SSRIs. However, they also found that high doses were associated with increased dropouts due to side effects (Simpson, 2020a).
To improve tolerability, patients should be started on low doses of medication for OCD. This can be increased every week or every other week (as tolerated). In addition, doses should be maintained within the therapeutic range for at least six weeks before concluding patients are resistant. The response curve of pharmacologic trials suggests that more than half of short-term improvement is evident by four weeks of treatment and more than three-quarters by six weeks with SSRIs (Simpson, 2020a).
A sufficient trial of SSRI for OCD is defined as the maximum dose tolerated for a minimum of six weeks. It is crucial to communicate with patients not to stop the medication before it has a chance to work (Simpson, 2020a).
Overall, clomipramine and SSRIs lead to improvement in 40-60% of individuals with OCD. In addition, patients who received a sufficient trial experienced a 20-40% reduction in symptoms. Therefore, these agents offer improvement rather than elimination of symptoms. There was no difference in efficacy among SSRIs (Simpson, 2020a).
There have been limited studies regarding serotonin and norepinephrine reuptake inhibitors (SNRIs). However, venlafaxine is the most widely studied, especially via randomized controlled trials (Yaryura-Tobias,1996):
Yaryura et al. compared venlafaxine vs. placebo and found no significant difference with symptoms of OCD.
Two other studies, which notably lacked placebos, compared higher doses of venlafaxine to clomipramine or SSRIs with similar response rates among these medications:
In a study by Albert et al., response rates were 36% for venlafaxine and 50% for clomipramine, according to the visit-wise analysis. In addition, response rates were 34.6% for venlafaxine and 42.6% for clomipramine, according to the last-observation-carried-forward analysis. Overall, there was no statistically significant difference between these medications. Of note, there was a much higher rate of adverse effects experienced by those taking clomipramine (Albert, 2002).
In a study by Denys et al., response rates for venlafaxine and paroxetine were approximately 40%. Patients on venlafaxine experienced a mean decrease of 7.2 ± 7.5 Y-BOCS, while those on paroxetine experienced a mean decrease of 7.8 ± 5.4 Y-BOCS. Overall, this study supported the use of venlafaxine as a safe, effective treatment compared to paroxetine for OCD (Denys, 2003).
Given that patients experience only partial relief from monotherapy with serotonergic medications, it makes sense that there would be interest in alternatives. Antipsychotics are effective in reducing symptoms in conjunction with clomipramine or SSRIs (Simpson, 2020a). In a meta-analysis by Dold et al., antipsychotics were more effective than placebo with augmentation of SSRIs. They improved the Y-BOCS total score with a Hedges's g of -0.64 and 95% confidence interval of -0.87 to -0.41 (Dold, 2015). In a retrospective study by Maina et al., they found a high risk of relapse from the discontinuation of antipsychotics with a mean worsening of symptoms of 6.6 ± 1.7 in the Y-BOCS total score (Maina, 2003).
Treatment of Pediatric Population
In a review of eleven case series encompassing hundreds of pediatric patients with OCD, the mean age of symptom onset was 10.3 years, while the mean age of assessment was 13 years, indicating a delay of several years between development and diagnosis. In contrast, the mean age of symptom onset for adults was 21 years, suggesting a bimodal distribution of incidence for OCD. Despite these similarities, there are differences in the phenotypic expression of this disorder depending on the age group. For example, children are more likely to display atypical rituals and compulsions without well-defined obsessions (Mancuso, 2010).
Though CBT is considered the first line of treatment for mild to moderate cases of pediatric OCD, severe cases may require the addition of pharmacotherapy. The POTS trial showed that combined treatment leads to the most significant decrease of symptoms and remission rates via effect sizes of CBT = 0.97, sertraline = 0.67, combined = 1.4. Due to variable potency and selectivity, it is difficult to predict how patients will respond to SSRIs. As a result, providers should decide based on adverse events and pharmacokinetic properties rather than efficacy (Mancuso, 2010).
A meta-analysis of various randomized controlled trials examining the use of medication to treat children and adolescents with this disorder showed a statistically significant difference between SSRIs and placebo for OCD with an effect size of 0.46 (Mancuso, 2010). In a separate systematic review and meta-analysis, they also found significant evidence supporting SSRIs over placebo with an effect size of 0.43 (Kotapati, 2019).
Treatment of Pregnancy/Postpartum Population
Data suggest that women are at high risk for the onset or exacerbation of this disorder immediately before and after birth. A systematic review indicated this was the case for childbearing outpatients during pregnancy (40%) and puerperium period (30%). In addition, a meta-analysis demonstrated a higher prevalence during pregnancy (2.07%) and postpartum period (2.43%). The exact cause is unknown, but research suggests this is due to fluctuations in estrogen, progesterone, or oxytocin. Untreated symptoms may have adverse effects on the mother and fetus/newborn (Namouz-Haddad, 2014).
Overall, CBT is considered the first line of treatment both in the general population and pregnant and postpartum women. If pharmacotherapy is indicated, the preferred medication is SSRIs. In refractory cases, atypical antipsychotics are used for augmentation. However, exposure to these medications during pregnancy is associated with an increased risk of spontaneous abortions, premature births, poor neonatal adaptation, and pulmonary hypertension of the newborn. Of note, no significant increase in major congenital malformations has been reported (Namouz-Haddad, 2014).
If treating a woman who is actively breastfeeding, counseling on the potential risks is necessary. Of the SSRIs, only fluoxetine was noted at relatively high levels in breast milk and could potentially lead to colic, drowsiness, and decreased weight gain (Namouz-Haddad, 2014).
Selective Serotonin Reuptake Inhibitors (SSRIs)
Fluoxetine
Mechanism of Action (FLUoxetine, 2020):
Fluoxetine inhibits the re-uptake of neuronal serotonin but has minimal or no effect on dopamine or norepinephrine. It has no significant affinity for muscarinic, histaminergic, or alpha-adrenergic receptors.
Dosage (FLUoxetine, 2020):
Adults:
Initial: 10-20mg/day; may increase by intervals of 20 mg/week
Recommended range: 40-80mg/day; may increase up to 120 mg/day x
Children (<7 years):
Initial: 5 mg/day
Children (≥7 years) and Adolescents:
Lower weight children:
Initial: 10mg/day
Daily dose: 20-30mg/day
Minimal experience with doses: >20mg/day
No experience with doses: >60mg/day
Higher weight children and adolescents:
Initial: 10mg/day; may increase by intervals of 20 mg/day after 2 weeks
Daily dose: 20-60mg/day
Geriatric:
See adult dosing
Blood Levels (Koran, 1996):
In a multicenter trial by Koran et al., it was found that plasma levels of fluoxetine and norfluoxetine are not related to clinical outcomes in patients with OCD. Plasma levels of those who responded to medication (decrease ≥50% in Y-BOCS score) did not differ significantly from those who did not respond (decrease ≤25% decrease in Y-BOCS score). Therefore, the optimum dose of fluoxetine is the most effective dose with the least side effect burden regardless of plasma levels.
Dosage for other SSRIs:
Citalopram (Lexicomp, 2021b):
Adults: 20-40mg/day
Children and adolescents:
Children (7 to ≤11 years): 10-40mg/day
Children and adolescents (≥12 years): 10-40mg/day
Geriatric: ≤20mg/day
Escitalopram (Lexicomp, 2021c)
Adults: 10-40mg/day
Children and adolescents: Efficacy not established
Geriatric: 10-20mg/day
Fluvoxamine (Lexicomp, 2021d)
Adults: 100-300mg/day
Children and adolescents (8 to 17 years): 50-200mg/day
Geriatric: See adult dosing
Paroxetine (Lexicomp, 2021e)
Adults: 40-60mg/day
Children and adolescents (7 to 17 years): 10-60mg/day
Geriatric: 10-40mg/day
Sertraline (Lexicomp, 2021g)
Adults: 50-200mg/day
Children and adolescents:
Children (6 to 12 years): 25-200mg/day
Adolescents (13 to 17 years): 25-200mg/day
Geriatric: See adult dosing
Tricyclic Antidepressants (TCAs)
Clomipramine
Mechanism of Action (ClomiPRAMINE, 2020):
Clomipramine inhibits the re-uptake of neuronal serotonin while its active metabolite, desmethylclomipramine, inhibits the re-uptake of neuronal norepinephrine.
Dosage (ClomiPRAMINE, 2020):
Adults
Initial: 25 mg/day; may increase up to 100 mg/day over 2 weeks
Maintenance: May increase up to 250 mg/day over several weeks
Children (≥10 years) and Adolescents:
Initial: 25 mg/day; may increase up to 3 mg/kg/day or 100 mg/day over 2 weeks (depending on whichever is less)
Maintenance: May increase up to 3 mg/kg/day or 200 mg/day over several weeks (depending on whichever is less)
Geriatric:
See adult dosing
Blood levels (Mavissakalian, 1990):
In a randomized controlled trial by Mavissakalian et al., it was found that plasma levels of clomipramine, but not any of its metabolites, were related to clinical outcomes in patients with OCD. Those who responded had significantly higher plasma levels of clomipramine.
Serotonin Norepinephrine Reuptake Inhibitors (SNRIs)
Venlafaxine
Mechanism of Action (Venlafaxine, 2020):
Venlafaxine and its active metabolite, O-desmethylvenlafaxine, inhibit re-uptake of neuronal serotonin and norepinephrine but have minimal effect on dopamine. They have no significant affinity for muscarinic, histaminergic, or alpha-adrenergic receptors.
Dosage (Lexicomp, 2020h):
Adults:
Initial: 75 mg/day; may increase by intervals of 75mg up to 225 mg/day over 2 weeks
Maintenance: May increase up to 350mg/day
Children and Adolescents:
Dose and efficacy not established
Geriatric:
See adult dosing
Antipsychotics
Aripiprazole
Mechanism of Action (de Bartolomeis, 2015):
Aripiprazole has high affinity for D2, D3, 5-HT1A, and 5-HT2A receptors and moderate affinity for D4, 5-HT2C, 5-HT7, alpha1 adrenergic, and H1 receptors. It also has moderate affinity for the serotonin reuptake transporter. It acts as a partial agonist at the D2 and 5-HT1A receptors and as an antagonist at the 5-HT2A receptor. It has no affinity for muscarinic receptors.
Dosage (Lexicomp, 2021a):
Adults:
Initial: 5mg/day
Maintenance: May increase by intervals of 5mg up to 15mg/day over ≥1 weeks
Children and Adolescents:
Dose and efficacy not established
Geriatric:
Dose and efficacy not established
Risperidone
Mechanism of Action (Lexicomp, 2021f):
Risperidone has low to moderate affinity for 5-HT1C, 5-HT1D and 5-HT1A receptors, weak affinity for D1 receptors, and no affinity for beta1, beta2, or muscarinic receptors. It acts as an antagonist at the 5-HT2 and dopamine-D2 receptors as well as alpha-adrenergic and histaminergic receptors.
Dosage (Lexicomp, 2021f):
Adults:
Initial: 0.25-0.5mg/day; may increase up to 0.5-1mg/day every 3 to 7 days
Maintenance: 0.5-2mg/day; may require dose up to 3mg/day
Children and Adolescents:
Dose and efficacy not established
Geriatric:
Dose and efficacy not established
Nonpharmacological Interventions
Brain Stimulation
Pharmacological interventions and cognitive behavioral therapy (CBT) are the first and second-line treatments for OCD. Despite the seeming multitude of options, 40-60% of patients with this disorder do not experience satisfactory responses. When faced with treatment resistance, it is necessary to consider alternative strategies (Saba, 2015).
Rapinesi et al. performed a systematic review of the effect of brain stimulation techniques for treatment-resistant OCD. Most research involves deep brain stimulation (DBS) and transcranial magnetic stimulation (TMS). There is less evidence regarding transcranial direct current stimulation (tDCS), electroconvulsive therapy (ECT), and vagus nerve stimulation (VNS). Overall, these treatments are promising as potential add-ons, but the results are inconsistent (Rapinesi, 2019):
TMS is a non-invasive technique that uses short magnetic pulses to modulate neural excitability via hyperpolarization or depolarization.
Rapinesi et al. found mixed results regarding the efficacy of TMS vs. sham-control studies in treatment-resistant OCD. The majority of the twenty studies did not demonstrate a significant difference between the variable and control conditions. However, one study showed this type of brain stimulation technique as an effective add-on treatment, two studies showed improvements in mood and movement urge, and four studies showed long-term symptom reduction.
DBS has been proposed as a last resort for patients who continue to display resistance to the treatment of OCD. It involves implanting electrodes within the brain and activating electrical stimulation of specific areas.
In the same systematic review, 53% of ventral capsule/ventral striatum or nucleus accumbens DBS and 41% subthalamic nucleus DBS displayed improvement in symptoms of OCD. Of note, the reduction of symptom severity threshold was poorly defined.
Other Neurosurgeries
Before the development of DBS, anterior capsulotomy was the traditional procedure for patients with refractory OCD. It specifically targeted the anterior limb of the internal capsule. In Pepper’s literature review of DBS vs. AC, 62% of patients who underwent AC experienced a clinically significant improvement compared with 52% of patients who received DBS; however, this difference was not statistically significant. In addition, patients treated with AC were more likely to go into remission than those treated with DBS (Pepper, 2015).
Neurofeedback
Neurofeedback is proposed as a non-chemical, non-invasive means of modulating brain function via real-time monitoring of the current brain state. It has been studied as a treatment modality for many disorders. However, there is little data regarding applicability for OCD (Rance, 2018).
A case series conducted by Surmeli et al. examined the efficacy of quantitative EEG-guided neurofeedback with drug-resistant OCD. 33 out of the 36 patients demonstrated clinical improvement as measured by the Y-BOCS, clinical global impression scale (CGI), and Minnesota Multiphasic Inventory (MMPI). The results support treatment with neurofeedback and encourage further research in this area (Surmeli, 2011).
Rance et al. studied the potential residual benefits of neurofeedback. They followed 17 patients after the intervention and determined maximum clinical outcomes occurred not immediately after but increased during the weeks following completion. The results were promising but require further inquiries to confirm these findings (Rance, 2018).
Cognitive Behavioral Therapy (CBT)
As mentioned previously, the leading treatments for this disorder are pharmacological interventions and cognitive behavioral therapy (CBT). CBT is not associated with adverse effects. Therefore, it is recommended as the first-line treatment before pharmacological interventions. Treatment includes psychoeducation, exposure and response prevention, and cognitive therapy (Abramowitz, 2019).
Psychoeducation: Before beginning treatment, the therapist must educate patients about the conceptual model of OCD. In addition, patients are informed about the process and benefits of CBT. Overall, psychoeducation prepares them for the distress and management of the following steps (Abramowitz, 2019).
Exposure and response prevention:
In vivo exposure: This involves helping the patient confront actual cues (e.g., words, objects, images, situations) known to trigger obsessions. These are presented hierarchically, progressing from least to most distressing (Foa, 2010).
Imaginal exposure: This involves asking the patient to imagine in detail the worst outcomes of their obsessions. The purpose is to encourage them to challenge the disastrous consequences they fear will result from failure to perform the rituals (Foa, 2010).
Ritual prevention: This involves instructing the patient to refrain from performing rituals they believe prevents feared outcomes or reduces distress. In this way, they learn that these goals can be accomplished without ritualizing (Foa, 2010).
Processing: This involves discussing the patient's experience with exposure and response prevention and if it confirmed or disconfirmed their expectations (Foa, 2010).
Cognitive therapy: Obsessions lead to distress because patients interpret them as warnings for likely and dangerous events. Cognitive therapy helps identify these unrealistic thoughts and challenge their interpretation. Patients are taught to develop an awareness of their obsessions and compulsions by keeping a "thought record." The therapist uses these entries in addition to gentle reasoning and Socratic questioning to verbally challenge their beliefs. They also initiate behavioral experiments to disprove any misconceptions about cause and effect. Over time, this helps patients acknowledge and eliminate their cognitive distortion (Foa, 2010).
CBT is indicated as a treatment for all levels of symptom severity with OCD. It is effective for most patients, but about 25-30% of drop out and 25% of those remaining do not show significant improvement. This form of therapy may not be as beneficial for patients who are developmentally disabled or cognitively impaired. Other populations less likely to benefit include those with comorbid depression, generalized anxiety disorder, psychosis, mania, or use of psychoactive substances (Abramowitz, 2019).
Another limiting factor with this treatment is the availability of specialists. The International Obsessive-Compulsive Disorder Foundation maintains a database of clinicians trained to utilize CBT for OCD.
Various studies have demonstrated the efficacy of CBT. When properly administered, it may lead to symptom reduction between 50-70%. A review of 12 trials found that 83% of patients with OCD responded to exposure-based CBT. A separate review of 16 studies showed that 76% of patients with OCD would continue to experience symptom reduction after completing CBT (Abramowitz, 2019).
A meta-analysis discovered additional relationships between CBT and treatment outcome with OCD (Abramowitz, 2019):
Patients demonstrate better short and long-term outcomes when exposure practice is supervised by a therapist rather than completed as homework outside of sessions.
Patients experience significant symptom reduction by combining imaginal and situational exposure.
Patients who refrain from engaging in rituals during treatment show immediate and superior long-term improvement (complete vs. partial response prevention).
Group Therapy
Group therapy is a standard modality utilized to treat mental illness and support people through various difficulties. Despite its known benefits, most evidence only exists for individual treatment regarding the efficacy of CBT in OCD. Fenger et al. performed a meta-analysis on several studies examining group therapy and naturalistic study on the effectiveness of their own treatment model (Fenger, 2007).
The meta-analysis examined 11 studies, five of which were conducted as randomized controlled studies. For most studies, total time in therapy was approximately two hours per week and took place one to two times per week (Fenger, 2007).
The randomized controlled trial studies examined cognitive-behavioral group therapy with a treatment duration of either 10 or 12 weeks. The mean pre-YBOCS score was 24.40, the mean post-YBOCS score was 16.02, and the mean effect size was 1.59 (Fenger, 2007):
One study compared patients in group therapy to patients receiving sertraline and weekly 20-minute visits and found no significant difference in symptom reduction. However, further analysis demonstrated that group therapy was linked to a significant reduction in compulsions and highest rate of symptom remission (Sousa, 2006).
Another study compared outcomes of weekly 1-hour individual sessions with weekly 2-hour group sessions (both used identical protocols) and found no significant difference (Anderson, 2007).
The other studies examined behavioral group therapy with a treatment duration of 7, 10, or 12 weeks. The mean pre-YBOCS score was 21.94, the mean post-YBOCS score was 15.48, and the mean effect size was 1.19 (Fenger, 2007).
The naturalistic study examined an original cognitive-behavioral group treatment with a treatment duration of 16 weeks. Y-BOCS, SCL-90-R, and GAF (Global Assessment of Functioning) were measured before and after the treatment, and patients improved significantly on all accounts. The mean pre-YBOCS score was 26.54, the mean post-YBOCS score was 20.40, and the mean effect size was 0.81 (Fenger, 2007).
Intensive CBT
The history of effective psychotherapy began with intensive behavioral therapy. Meyer et al. is credited with one of the first breakthroughs after successfully treating two inpatients with OCD. The treatment involved exposure and response prevention for 3-4 weeks with gradual withdrawal of supervision, restrictions, and therapy sessions. Patients spent 9 and 12 weeks in the hospital with 25 and 20 therapy hours (Jonsson, 2015).
Over time, this intensive format was adjusted to weekly or, at most, twice weekly. However, it can still be advantageous or preferred for patients who have severe symptoms or require rapid improvement. It could also be used for those who work or study (Jonsson, 2015).
Jonsson et al. performed a meta-analysis that found intensive CBT is an effective treatment for children, adolescents, and adults with OCD (Jonsson, 2015):
17 trials (11 adult and 6 youth) with a total of 646 patients:
Four randomized controlled trials, four controlled studies, and nine naturalistic studies
Intensive CBT was defined as:
Individual treatment: Maximum 4 weeks
Weekly therapist hours: Minimum 5 hours
Total therapist hours: Minimum 20 hours
Pre-post effect sizes of 2.44 (95% CI 2.03-2.85) for clinical ratings (n=16) and 1.23 (95% CI 1.01-1.45) for self-reports (n=5)
Other Psychotherapies
CBT is considered more efficacious than other psychosocial interventions, including progressive muscle relaxation and anxiety management training. There have been no randomized controlled trials examining psychodynamic psychotherapy or eclectic psychotherapy to treat OCD (Abramowitz, 2019).
The Four Steps Approach
Adapted from Brain Lock: Free Yourself From Obsessive-Compulsive Behavior
By Dr. Jeffrey M. Schwartz
The Four Steps is a self-directed cognitive-behavioral therapy technique developed by Schwartz and his team to supplement and enhance the process of exposure and response prevention. Although it was designed to help patients guide their own behavior therapy, it can also readily be done with a therapist (Schwartz, 2016).
Mindful Awareness:
In the context of this book, “mindful awareness” is described as the ability to recognize obsessions as false messages. It requires the patient to recognize and acknowledge the unpleasant feelings associated with OCD. Schwartz personifies this term by referencing a philosophical concept of “the impartial and well-informed spectator,” which he later calls the “impartial spectator.” In other words, it is the capacity to be fully aware of situations and feelings while maintaining impartiality. While practicing “mindful awareness,” patients will find that the mere observation of the obsessive thoughts helps to decrease the associated frequency and distress (Schwartz, 2016).
The Four Steps:
1. Relabel:
With relabeling, patients are encouraged to identify the intrusive thought or urge to perform a compulsion for precisely what it is– an obsessive thought or compulsive urge. With this step, it is essential to utilize the ability of the “impartial spectator” as it allows patients to look outside themselves and observe their actions with “mindful awareness.” It is designed to help patients distinguish between their disorder and true desires. Schwartz uses obsessive hand washing as an example. Instead of saying, “I feel like I need to wash my hands again, even though I know it doesn’t make any sense,” the patient can say, “I am having a compulsive urge. That compulsion is bothering me. That obsessive thought is hounding me” (Schwartz, 2016).
2. Reattribute:
Reattributing means answering the question why do obsessive thoughts or compulsive urges keep occurring? The answer is because of OCD. Patients are reminded that their disorder results from biochemical imbalances in the brain that interfere with its ability to “switch gears.” Because it gets “stuck in gear,” the “error-detection circuit” continues to fire inappropriately, leading to distressing feelings. As patients modify their behavior and “gearshift” becomes “unstuck,” the discomfort will begin to fade (Schwartz, 2016).
3. Refocus:
When appropriate, refocusing addresses what can be done to overcome compulsive urges. Instead of taking obsessions and compulsions at face value, patients are encouraged to keep in mind that these are false messages. They can learn to ignore or avoid by refocusing their attention toward different behaviors. For example, they can utilize the “fifteen-minute rule” by engaging in an enjoyable or productive activity for at least fifteen minutes. Afterward, patients are instructed to note how their symptoms have changed and then repeat the process. They are also encouraged to practice being an “impartial spectator” while refocusing. Dr. Schwartz refers to this as “shifting gears” (Schwartz, 2016).
4. Revalue:
Lastly, revaluing teaches patients how to devalue their obsessive thoughts and compulsive urges as worthless. This step involves the two subsets of “relabel” and “reattribute:” “the two A’s” – anticipate and accept. The first “A” encourages patients to anticipate obsessive thoughts in preparation for the Four Steps. The second “A” reminds patients to accept that their disorder is a medical condition rather than a character flaw (Schwartz, 2016).
Common Psychotherapy Mistakes
Although the principle of exposure and response prevention seems straightforward (exposure to obsession-provoking stimuli and refraining from compulsive behaviors), actual practice is more complicated. Thus, inexperienced or improperly trained therapists are at risk of making errors that interfere with the exposure component, response component, or both. Common mistakes are as follows (Gillihan, 2012):
Not encouraging patients to push hard enough in exposures
Exposure and response prevention therapy must thoroughly address the avoidance and rituals that patients falsely believe prevent the occurrence of feared outcomes. The purpose is to maximize invalidation of the obsessional thought to decrease the chances of attributing effectiveness to compulsive urges. Untreated areas make relapse more likely during the process of recovery. As a result, patients need to know, even though the goal is to help them live a normal life, treatment will involve going beyond what would be considered “normal” by people without OCD. Therapists must ensure patients understand this concept, emphasize the importance of completing exposures, and encourage overstepping comfort zones.
Employing an inappropriate form of exposure
As mentioned previously, there are two forms of exposure: in vivo and imaginal exposure.
In vivo exposure involves patients facing actual stimuli or situations associated with their obsessions. There are several potential mechanisms as to why this leads to symptom relief. First, it allows direct and robust invalidation of feared outcomes. In addition, it helps patients understand that their distress is not indefinite but manageable.
Imaginal exposure instructs patients to develop a narrative as vividly as possible about the worst outcome of their obsession-related fears. In order for the exposure to be effective, distress must be monitored to ensure appropriate anxiety levels. It is essential to repeat these imaginary scenarios for multiple reasons. First, repeated exposure disproves the belief that confronting obsessions is always distressing. Second, patients learn that fixating on these imaginary scenarios does not bring their fears to fruition. Third, it decreases distress and encourages reappraisal of the likelihood of the feared outcome.
Of note, it is essential to conduct in vivo exposure in addition to imaginal exposure. It is difficult for patients to draw the same conclusions with imaginal exposure as experienced within vivo exposure. In this way, patients may be tempted to attribute the lack of fear outcomes to the absence of actual stimuli or situations.
Promoting distraction during exposure
It is important to be aware of the subtle forms of avoidance during exposure and response prevention therapy. There is debate about the effect of distraction during treatment. However, attention to the obsessional and compulsive content is essential for therapeutic outcomes. Distraction can be beneficial if it facilitates the completion of exposures and disconfirmation of fears. On the other hand, it can also undermine treatment if the patient dedicates too much mental energy or believes the feared outcome did not occur because of the distraction. Lastly, patients may use distraction to subtly or intentionally distance themselves from the exposure. The therapist needs to be attentive to the patient in order to redirect them if necessary.
Giving patients reassurance
Patients often feel the need to be reassured with their obsessions. Most therapists have been trained to reassure patients as appropriate, especially early in the treatment process. For example, a patient with fears of being a child molester who has no inappropriate interest in children can be reassured about the role of OCD. Unfortunately, too much reassurance can be counterproductive by dampening exposure to the actual stimuli or situation and sparing the patient from having to cope with degrees of uncertainty. During therapy, clinicians should explain that requests for assurance will be denied to discourage patients from seeking reassurance. In addition, any praise should be directed towards engaging exposures.
Treating peripheral symptoms instead of the core fear
In the planning stages of exposure and response therapy, the therapist and patient create a hierarchy of exposures intended to trigger distress. During this process, there is an abundance of rituals stemming from a few or even single “core fear.” For example, an individual with obsessions and compulsions associated with religion or morality might have a core fear of eternal damnation. Potential branching rituals include repeating prayers, avoiding demonic numbers, and redoing actions if initially performed while thinking about Satan.
Identifying the core fears and designing a specific exposure allows for a faster and comprehensive therapeutic effect as well as decreased risk of relapse. Even if rituals on the exposure hierarchy are addressed superficially, the patient may still successfully become sensitized to them and other similar triggers. However, proceeding without the core fear is likely to yield slower and limited results. In addition, there is the possibility of other rituals replacing the ones that were eliminated.
For many core fears, the combination of in vivo and imaginal exposure gives rise to the best outcomes. Habituation to the consequences of core fears facilitates the elimination of avoidance and rituals leading to decreased distress that n generalizes downward to triggers. Of note, not all patients need imaginal exposure. In addition, some may not even have core fears. Regardless, it is crucial to thoroughly and collaboratively investigate fears and rituals to verify the lack of a core fear.
Ineffectively addressing mental compulsions
Mental compulsions involve words, phrases, numbers, images, or prayers that patients repeat to themselves in order to alleviate anxiety or prevent a feared outcome. Unfortunately, these are more likely to be missed or mistaken for obsessions. It is important to understand that the form of obsessions and compulsions may be the same, but the function is quite different. Obsessions are intrusive thoughts that increase distress, while mental compulsions are almost involuntary acts that decrease distress. It may be necessary to have patients replace these with exposure statements targeting their core fear. If and when patients perform mental compulsions, therapists should teach them to re-expose themselves to the triggering stimulus.
Neglecting to work with and/or teach patients’ loved ones
Many patients with this disorder recruit loved ones to participate in their compulsions. For example, family members or friends may agree to clean the house, so the patient does not have to experience any distress associated with contamination. Given these possibilities, it is necessary to encourage patients to refrain from seeking reassurance and instruct loved ones how to respond in these situations. This includes clarifying the reason and importance of discouraging obsessions and compulsions as well as teaching how to differentiate between providing reassurance vs. comfort and support. If patients continue to look to press their loved ones despite them responding appropriately, the targeted individual should be encouraged to exit the encounter or respond with an exposure statement that targets the core fear.
Barriers and Gateways to Successful Psychotherapy
Relapses
OCD can be a lifelong disorder with the potential for relapse. However, this does not mean that patients cannot have fulfilling lives; instead, they must be vigilant and recognize that recovery is an active process. While relapses are normal, they should be prepared and ready to get back on track immediately (Penzel, 2000).
Patients need to understand that they cannot keep living the same way if they hope to improve. Living a balanced life is essential, including getting adequate sleep, eating a healthy diet, engaging in regular exercise, having a community and social life, maintaining close friendships and intimate relationships, being employed in a productive setting, and seeing health professionals for addressing problems and regular check-ups (Penzel, 2000).
In accordance with a balanced life, patients must also strive to live less rigidly, and introducing flexibility and variety helps create an environment conducive to recovery (Penzel, 2000).
It is essential for expectations for post-recovery life to be realistic. Patients must learn to tolerate their need for certainty and perfection. They must also acknowledge and accept that struggling will be inevitable (Penzel, 2000).
At the same time, adjusting to life in recovery will allow them to fully and actively participate in the same environment as before, but this time with more techniques and tools to manage their obsessions and compulsions (Penzel, 2000).
Acceptance
Although many patients have access to the same information and resources, not everyone experiences change, and acceptance seems to be the determining factor. In the context of OCD, patients must accept that recovery will be difficult and discouraging. Of importance, acceptance does not mean enjoying the process (Penzel, 2000).
Penzel defines acceptance as “a willingness to unconditionally undergo every part of the struggle for recovery, including negative feelings such as anxiety, and despite the possibility that setbacks and pain may result” (Penzel, 2000).
Some obstacles to acceptance are (Penzel, 2000):
Irrational demandingness: Insistence that recovery should not be challenging or the disorder should not exist.
Denial: Rejecting the reality of having the disorder.
Distortion: Minimizing the effect of the disorder.
Avoidance: Acknowledging the existence of the disorder but refusing to face it.
Procrastination: Acknowledging the existence of the disorder but choosing to address it later.
Perfectionism: Having no tolerance for anything being less than 100%.
Cultural influences: “Can-do” or “just do it” culture that teaches the sources of our problems can be modified or removed.
Penzel lists several facets of acceptance that assist in recovery. They are referred to as The Five Acceptances and are as follows (Penzel, 2000):
Accept yourself
Patients should not define themselves by their disorder or reduce existence to a single aspect of life. OCD is not their fault and does not make them any more imperfect than other human beings.
Accept others
It is important to remember that other people are also imperfect. In this way, it is not fair for patients to demand perfection of their community with providing support or understanding OCD.
Accept the illness and the nature of the illness
Due to the nature of this disorder, patients will experience unpleasant obsessions and compulsions. They will also retain a tendency toward this disorder even during recovery.
Accept the nature of the task of therapy
It is the patient’s responsibility to seek help and do the work of therapy. Especially at the beginning, it will often involve tasks that seem risky and impossible. It is important to remember that this process will take time and not without errors or relapses.
Accept the nature of the task of ongoing recovery
Recovery means that patients have their symptoms under control and can function more fully. Setbacks should be addressed immediately but not be viewed as relapses. It is important to avoid “all-or-nothing” thinking because these do not indicate weakness or incapability. In addition, patients should try to avoid internalizing a false concept of willpower based on the idea that having this disorder is due to a character flaw. This process is a journey, not a destination.
Grief During Recovery
Although the degree of disability will vary, many patients will experience a spectrum of loss due to having OCD. As a result, it is necessary to explore how patients can make sense of their disorder and have fulfilling lives in light of this reality. They may likely have a sense of grief, and problems can arise during treatment and recovery if unresolved. Working towards a normal life involves more than controlling symptoms (Penzel, 2000).
Some patients may achieve this healing on their own, but some may need assistance. There are various reasons for this, but the most significant is lack of social support. Penzel quotes Dr. J. William Worden from Grief Counseling and Grief Therapy, saying, “Grief is really a social process and is best dealt with in a social setting in which people can support and reinforce each other in reaction to the loss.” Patients talking openly and honestly about their losses is undeniable while working through grief (Penzel, 2000).
Loss due to a psychological disorder is not simple or easy to share with other people. It might involve revealing the existence of the disorder and risking rejection as a result. Furthermore, it is possible that those available to talk may not view this loss seriously or refuse to acknowledge it even occurred. In these situations, support groups and additional therapy may be beneficial. Given that grief is part of this disorder, the goals of grief therapy are applicable and are as follows (Penzel, 2000):
First, patients need to accept the reality of the loss and imperfections of life.
Second, the pain must be addressed in the open, examined, and released by sharing with other people to take away the power and pain of this disorder.
Third, it is necessary to establish a new sense of self and normalize loss.
Fourth, the emotional energy must be redirected to move forward with life.
Paradoxically, some people go through a period of grieving this disorder itself after recovery. A feeling of emptiness can arise, especially when their symptoms have been such a prominent aspect of their lives. Fortunately, this can be addressed by occupying their time with positive actions (Schwartz, 2016).
It will be evident that these milestones have been reached when the patient can think of the loss without pain, experience the joys of life, reinvest in emotions, adjust to new roles, and work toward a better future (Penzel, 2000).
Transitioning and Life Skills
Due to the nature of symptoms, many aspects of life may fall by the wayside for individuals with OCD. This can lead to unfamiliarity with what it means to live functionally rather than dysfunctionally. Of course, there is variation from patient to patient. Those with adult-onset or mild to moderate symptoms may have many unaffected years and function close to normal. On the other hand, those with childhood or adolescent-onset or severe symptoms may struggle to understand life without OCD (Penzel, 2000).
The process of recovery may feel overwhelming and anxiety-provoking. It is crucial to support patients in gradually re-entering environments and activities such as school, work, or relationships (Penzel, 2000).
Media Portrayal
Movie Clips Portraying OCD:
As Good as it Gets (1997):
3 minute movie clip displaying character performing excessive and ritualistic counting and cleaning behaviors
Matchstick Men (2003):
3 minute movie clip displaying character counting, cleaning, and checking with evident distress while relaying experience to therapist
1 minute movie clip displaying character exhibiting vocal and physical tics
The Aviator (2004):
3 minute movie clip displaying character hand washing to the point of self-injury along with inability to open doors due to fear of contamination
Sources
Abramowitz, Jonathan. (2019). Psychotherapy for obsessive-compulsive disorder in adults. UptoDate.
Retrieved March 11, 2021, from https://www.uptodate.com/contents/psychotherapy-for-obsessive-compulsive-disorder-in-adults?search=psychotherapy-for-obsessive-comulsion-disorder-in-adults&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
Albert, U., Aguglia, E., Maina, G., & Bogetto, F. (2002). Venlafaxine versus clomipramine in the treatment of
obsessive-compulsive disorder: a preliminary single-blind, 12-week, controlled study. The Journal of clinical psychiatry, 63(11), 1004–1009. https://doi.org/10.4088/jcp.v63n1108
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
https://doi.org/10.1176/appi.books.9780890425596
Anderson, R. A., & Rees, C. S. (2007). Group versus individual cognitive-behavioural treatment for
obsessive-compulsive disorder: a controlled trial. Behaviour research and therapy, 45(1), 123–137. https://doi.org/10.1016/j.brat.2006.01.016
Bottas, A., Cooke, R. G., & Richter, M. A. (2005). Comorbidity and pathophysiology of obsessive-compulsive disorder
in schizophrenia: is there evidence for a schizo-obsessive subtype of schizophrenia?. Journal of psychiatry & neuroscience : JPN, 30(3), 187–193.
Brennan, B. P., Rauch, S. L., Jensen, J. E., & Pope, H. G., Jr (2013). A critical review of magnetic resonance
spectroscopy studies of obsessive-compulsive disorder. Biological psychiatry, 73(1), 24–31. https://doi.org/10.1016/j.biopsych.2012.06.023
ClomiPRAMINE. (2020, July 30). Drugs.com. Retrieved July 20, 2020, from
https://www.drugs.com/ppa/clomipramine.html
de Bartolomeis, A., Tomasetti, C., & Iasevoli, F. (2015). Update on the Mechanism of
Action of Aripiprazole: Translational Insights into Antipsychotic Strategies Beyond
Dopamine Receptor Antagonism. CNS drugs, 29(9), 773–799. https://doi.org/10.1007/s40263-015-0278-3
Denys, D., van der Wee, N., van Megen, H. J., & Westenberg, H. G. (2003). A double blind comparison of
venlafaxine and paroxetine in obsessive-compulsive disorder. Journal of clinical psychopharmacology, 23(6), 568–575. https://doi.org/10.1097/01.jcp.0000095342.32154.54
Dold, M., Aigner, M., Lanzenberger, R., & Kasper, S. (2015). Antipsychotic Augmentation of Serotonin Reuptake
Inhibitors in Treatment-Resistant Obsessive-Compulsive Disorder: An Update Meta-Analysis of Double-Blind, Randomized, Placebo-Controlled Trials. The international journal of neuropsychopharmacology, 18(9), pyv047. https://doi.org/10.1093/ijnp/pyv047
Fenger, M. M., Mortensen, E. L., Rasmussen, J., & Lau, M. (2007). Group therapy with OCD: Development and
outcome of diagnosis specific treatment of patients with OCD in groups. Nordic Psychology, 59(4), 332–346. https://doi.org/10.1027/1901-2276.59.4.332
FLUoxetine. (2020, July 9). Drugs.com. Retrieved July 20, 2020, from https://www.drugs.com/ppa/fluoxetine.html
Foa E. B. (2010). Cognitive behavioral therapy of obsessive-compulsive disorder. Dialogues in clinical neuroscience,
12(2), 199–207. https://doi.org/10.31887/DCNS.2010.12.2/efoa
Fornaro, M., Gabrielli, F., Albano, C., Fornaro, S., Rizzato, S., Mattei, C., Solano, P., Vinciguerra, V., & Fornaro, P.
(2009). Obsessive-compulsive disorder and related disorders: a comprehensive survey. Annals of general psychiatry, 8, 13. https://doi.org/10.1186/1744-859X-8-13
Geller, D. A., & March, J., (2012). Practice parameter for the assessment and treatment of children and adolescents
with obsessive-compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 51(1), 98-113. https://doi.org/10.1016/j.jaac.2011.09.019
Gillihan, S. J., Williams, M. T., Malcoun, E., Yadin, E., & Foa, E. B. (2012). Common Pitfalls in Exposure and
Response Prevention (EX/RP) for OCD. Journal of obsessive-compulsive and related disorders, 1(4), 251–257. https://doi.org/10.1016/j.jocrd.2012.05.002
Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleischmann, R. L., Hill, C. L., Heninger, G. R., &
Charney, D. S. (1989). The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Archives of general psychiatry, 46(11), 1006–1011. https://doi.org/10.1001/archpsyc.1989.01810110048007
Grant J. E. (2014). Clinical practice: Obsessive-compulsive disorder. The New England journal of medicine, 371(7),
646–653. https://doi.org/10.1056/NEJMcp1402176
Grassi, G., Poli, L., Cantisani, A., Righi, L., Ferrari, G., & Pallanti, S. (2014). Hypochondriasis and
obsessive-compulsive disorder in schizophrenic patients treated with clozapine vs other atypical antipsychotics. CNS spectrums, 19(4), 340–346. https://doi.org/10.1017/S1092852913000795
Grisham, J. R., Fullana, M. A., Mataix-Cols, D., Moffitt, T. E., Caspi, A., & Poulton, R. (2011). Risk factors
prospectively associated with adult obsessive-compulsive symptom dimensions and obsessive-compulsive disorder. Psychological medicine, 41(12), 2495–2506. https://doi.org/10.1017/S0033291711000894
Hershfield, J., Corboy, T. (2014). Mindfulness workbook for OCD: A guide to overcoming obsessions and
compulsions using mindfulness and cognitive behavioral therapy. New Harbinger Publications.
Heyman, I., Mataix-Cols, D., & Fineberg, N. A. (2006). Obsessive-compulsive disorder. BMJ (Clinical research ed.),
333(7565), 424–429. https://doi.org/10.1136/bmj.333.7565.424
Hilker, R., Helenius, D., Fagerlund, B., Skytthe, A., Christensen, K., Werge, T. M., Nordentoft, M., & Glenthøj, B. (
2018). Heritability of Schizophrenia and Schizophrenia Spectrum Based on the Nationwide Danish Twin Register. Biological psychiatry, 83(6), 492–498. https://doi.org/10.1016/j.biopsych.2017.08.017
Johansson, V., Kuja-Halkola, R., Cannon, T. D., Hultman, C. M., & Hedman, A. M. (2019). A population-based
heritability estimate of bipolar disorder - In a Swedish twin sample. Psychiatry research, 278, 180–187. https://doi.org/10.1016/j.psychres.2019.06.010
Jónsson, H., Kristensen, M., & Arendt, M. (2015). Intensive cognitive behavioural therapy for obsessive-compulsive
disorder: A systematic review and meta-analysis. Journal of Obsessive-Compulsive and Related Disorders, 6, 83–96. https://doi.org/10.1016/j.jocrd.2015.04.004
Koran, L. M., Cain, J. W., Dominguez, R. A., Rush, A. J., & Thiemann, S. (1996). Are fluoxetine plasma levels related
to outcome in obsessive-compulsive disorder?. The American journal of psychiatry, 153(11), 1450–1454. https://doi.org/10.1176/ajp.153.11.1450
Kotapati, V. P., Khan, A. M., Dar, S., Begum, G., Bachu, R., Adnan, M., Zubair, A., & Ahmed, R. A. (2019). The
Effectiveness of Selective Serotonin Reuptake Inhibitors for Treatment of Obsessive-Compulsive Disorder in
Adolescents and Children: A Systematic Review and Meta-Analysis. Frontiers in psychiatry, 10, 523. https://doi.org/10.3389/fpsyt.2019.00523
Krebs, G. C., Hannigan, L. J., Gregory, A. M., Rijsdijk, F. V., Maughan, B., & Eley, T. C. (2019). Are punitive parenting
and stressful life events environmental risk factors for obsessive-compulsive symptoms in youth? A longitudinal twin study. European psychiatry : the journal of the Association of European Psychiatrists, 56, 35–42. https://doi.org/10.1016/j.eurpsy.2018.11.004
Lexicomp. (2021a) Aripiprazole: Drug Information. UpToDate. Retrieved May 31, 2021, from
Lexicomp. (2021b) Citalopram: Drug Information. UpToDate. Retrieved May 22, 2021, from
esult&selectedTitle=1~101&usage_type=panel&kp_tab=drug_general&display_rank=1
Lexicomp. (2021c) Escitalopram: Drug Information. UpToDate. Retrieved May 22, 2021, from
Lexicomp. (2021d) Fluvoxamine: Drug Information. UpToDate. Retrieved May 22, 2021, from
Lexicomp. (2021e) Paroxetine: Drug Information. UpToDate. Retrieved May 22, 2021, from
Lexicomp. (2021f) Risperidone: Drug Information. UpToDate. Retrieved May 31, 2021, from
Lexicomp. (2021g) Sertraline: Drug Information. UpToDate. Retrieved May 22, 2021, from
Lexicomp. (2021h) Venlafaxine: Drug Information. UpToDate. Retrieved May 31, 2021, from
Lochner, C., Seedat, S., du Toit, P. L., Nel, D. G., Niehaus, D. J., Sandler, R., & Stein, D. J. (2005).
Obsessive-compulsive disorder and trichotillomania: a phenomenological comparison. BMC psychiatry, 5, 2. https://doi.org/10.1186/1471-244X-5-2
Maina, G., Albert, U., Ziero, S., & Bogetto, F. (2003). Antipsychotic augmentation for treatment resistant
obsessive-compulsive disorder: what if antipsychotic is discontinued?. International clinical psychopharmacology, 18(1), 23–28. https://doi.org/10.1097/00004850-200301000-00004
Mancuso, E., Faro, A., Joshi, G., & Geller, D. A. (2010). Treatment of pediatric obsessive-compulsive disorder: a
review. Journal of child and adolescent psychopharmacology, 20(4), 299–308. https://doi.org/10.1089/cap.2010.0040
Mataix-Cols D. (2014). Clinical practice. Hoarding disorder. The New England journal of medicine, 370(21),
2023–2030. https://doi.org/10.1056/NEJMcp1313051
Mavissakalian, M. R., Jones, B., Olson, S., & Perel, J. M. (1990). Clomipramine in obsessive-compulsive disorder:
clinical response and plasma levels. Journal of clinical psychopharmacology, 10(4), 261–268.
Namouz-Haddad, S., & Nulman, I. (2014). Safety of treatment of obsessive compulsive disorder in pregnancy and
puerperium. Canadian family physician Medecin de famille canadien, 60(2), 133–136.
Nikolas, M. A., & Burt, S. A. (2010). Genetic and environmental influences on ADHD symptom dimensions of
inattention and hyperactivity: a meta-analysis. Journal of abnormal psychology, 119(1), 1–17. https://doi.org/10.1037/a0018010
Oberbeck, A., Stengler, K., & Steinberg, H. (2013). Die Geschichte der Zwangserkrankung: Ihre Stellung im Wandel
der psychiatrischen Formenlehre bis Anfang des 20. Jahrhunderts [On the history of obsessive compulsive disorders: their place in the nosological classifications up to the beginning of the 20th century]. Fortschritte der Neurologie-Psychiatrie, 81(12), 706–714. https://doi.org/10.1055/s-0033-1355702
Parmar, A., & Sarkar, S. (2016). Neuroimaging Studies in Obsessive Compulsive Disorder: A Narrative Review.
Indian journal of psychological medicine, 38(5), 386–394. https://doi.org/10.4103/0253-7176.191395
Pauls D. L. (2010). The genetics of obsessive-compulsive disorder: a review. Dialogues in clinical neuroscience,
12(2), 149–163. https://doi.org/10.31887/DCNS.2010.12.2/dpauls
Penzel, F. (2000). Obsessive-compulsive disorders: A complete guide to getting well and staying well. Oxford
University Press.
Pepper, J., Hariz, M., & Zrinzo, L. (2015). Deep brain stimulation versus anterior capsulotomy for
obsessive-compulsive disorder: a review of the literature. Journal of neurosurgery, 122(5), 1028–1037.
https://doi.org/10.3171/2014.11.JNS132618
Pitman R. K. (1987). Pierre Janet on obsessive-compulsive disorder (1903). Review and commentary. Archives of
general psychiatry, 44(3), 226–232. https://doi.org/10.1001/archpsyc.1987.01800150032005
Rance, M., Walsh, C., Sukhodolsky, D. G., Pittman, B., Qiu, M., Kichuk, S. A., Wasylink, S., Koller, W. N., Bloch, M.,
Gruner, P., Scheinost, D., Pittenger, C., & Hampson, M. (2018). Time course of clinical change following neurofeedback. NeuroImage, 181, 807–813. https://doi.org/10.1016/j.neuroimage.2018.05.001
Rapinesi, C., Kotzalidis, G. D., Ferracuti, S., Sani, G., Girardi, P., & Del Casale, A. (2019). Brain Stimulation in
Obsessive-Compulsive Disorder (OCD): A Systematic Review. Current neuropharmacology, 17(8), 787–807. https://doi.org/10.2174/1570159X17666190409142555
Richter, P., & Ramos, R. T. (2018). Obsessive-Compulsive Disorder. Continuum (Minneapolis, Minn.), 24(3,
BEHAVIORAL NEUROLOGY AND PSYCHIATRY), 828–844. https://doi.org/10.1212/CON.0000000000000603
Rosenberg, David. (2019). Obsessive-compulsive disorder in children and adolescents: Epidemiology, pathogenesis,
clinical manifestations, course, assessment, and diagnosis. Retrieved March 28, 2021, from
y-pathogenesis-clinical-manifestations-course-assessment-and-diagnosis?search=ego%20dystonic&source
=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
Ruscio, A. M., Stein, D. J., Chiu, W. T., & Kessler, R. C. (2010). The epidemiology of obsessive-compulsive disorder
in the National Comorbidity Survey Replication. Molecular psychiatry, 15(1), 53–63.
https://doi.org/10.1038/mp.2008.94
Saba, G., Moukheiber, A., & Pelissolo, A. (2015). Transcranial cortical stimulation in the treatment of
obsessive-compulsive disorders: efficacy studies. Current psychiatry reports, 17(5), 36. https://doi.org/10.1007/s11920-015-0571-3
Scahill, L., Riddle, M. A., McSwiggin-Hardin, M., Ort, S. I., King, R. A., Goodman, W. K., Cicchetti, D., & Leckman, J.
F. (1997). Children's Yale-Brown Obsessive Compulsive Scale: reliability and validity. Journal of the
American Academy of Child and Adolescent Psychiatry, 36(6), 844–852. https://doi.org/10.1097/00004583-199706000-00023
Schwartz, J. M. (2016). Brain lock: Free yourself from obsessive-compulsive behavior. HarperCollins.
Silventoinen, K., Sammalisto, S., Perola, M., Boomsma, D. I., Cornes, B. K., Davis, C., Dunkel, L., De Lange, M.,
Harris, J. R., Hjelmborg, J. V., Luciano, M., Martin, N. G., Mortensen, J., Nisticò, L., Pedersen, N. L., Skytthe, A., Spector, T. D., Stazi, M. A., Willemsen, G., & Kaprio, J. (2003). Heritability of adult body height: a comparative study of twin cohorts in eight countries. Twin research : the official journal of the International Society for Twin Studies, 6(5), 399–408. https://doi.org/10.1375/136905203770326402
Simpson Blair, Helen. (2020a) Pharmacotherapy for obsessive-compulsive disorder in adults. UptoDate. Retrieved
https://www.uptodate.com/contents/pharmacotherapy-for-obsessive-compulsive-disorder-in-adults
Simpson Blair, Helen. (2020b). Obsessive-compulsive disorder in adults: Epidemiology, pathogenesis, clinical
manifestations, course, and diagnosis. UptoDate. Retrieved June 1, 2020, from
Skodol, Andrew. (2018) Overview of personality disorders. UptoDate. Retrieved March 28, 2021, from
Skoglund, C., Tiger, A., Rück, C., Petrovic, P., Asherson, P., Hellner, C., Mataix-Cols, D., & Kuja-Halkola, R. (2021).
Familial risk and heritability of diagnosed borderline personality disorder: a register study of the Swedish population. Molecular psychiatry, 26(3), 999–1008. https://doi.org/10.1038/s41380-019-0442-0
Sousa, M. B., Isolan, L. R., Oliveira, R. R., Manfro, G. G., & Cordioli, A. V. (2006). A randomized clinical trial of
cognitive-behavioral group therapy and sertraline in the treatment of obsessive-compulsive disorder. The Journal of clinical psychiatry, 67(7), 1133–1139. https://doi.org/10.4088/jcp.v67n0717
Stein, D. J., Fineberg, N. A., Bienvenu, O. J., Denys, D., Lochner, C., Nestadt, G., Leckman, J. F., Rauch, S. L., &
Phillips, K. A. (2010). Should OCD be classified as an anxiety disorder in DSM-V?. Depression and anxiety, 27(6), 495–506. https://doi.org/10.1002/da.20699
Steketee, G., Frost, R., & Bogart, K. (1996). The Yale-Brown Obsessive Compulsive Scale: interview versus
self-report. Behaviour research and therapy, 34(8), 675–684. https://doi.org/10.1016/0005-7967(96)00036-8
Sürmeli, T., & Ertem, A. (2011). Obsessive compulsive disorder and the efficacy of qEEG-guided neurofeedback
treatment: a case series. Clinical EEG and neuroscience, 42(3), 195–201. https://doi.org/10.1177/155005941104200310
van Grootheest, D. S., Cath, D. C., Beekman, A. T., & Boomsma, D. I. (2005). Twin studies on obsessive-compulsive
disorder: a review. Twin research and human genetics : the official journal of the International Society for Twin Studies, 8(5), 450–458. https://doi.org/10.1375/183242705774310060
Veale, D., & Roberts, A. (2014). Obsessive-compulsive disorder. BMJ (Clinical research ed.), 348, g2183.
https://doi.org/10.1136/bmj.g2183
Venlafaxine. (2020, June 1). Drugs.com. Retrieved July 20, 2020, from https://www.drugs.com/pro/venlafaxine.html
Woody, S. R., Steketee, G., & Chambless, D. L. (1995). Reliability and validity of the Yale-Brown
Obsessive-Compulsive Scale. Behaviour research and therapy, 33(5), 597–605. https://doi.org/10.1016/0005-7967(94)00076-v
Yaryura-Tobias, J. A., & Neziroglu, F. A. (1996). Venlafaxine in obsessive-compulsive disorder. Archives of general
psychiatry, 53(7), 653–654. https://doi.org/10.1001/archpsyc.1996.01830070103016
Acknowledgements:
This article was supported by “Mental Health Education & Research”.