Episode 104: Psilocybin Therapy Part 1: History, Pop Culture, Safety and Side Effects, MDMA Studies, And Early Research
By listening to this episode, you can earn 1.75 Psychiatry CME Credits.
Other Places to listen: iTunes, Spotify
Article Authors: Nadav Klein MD, David Puder, MD
We have no conflicts of interest to report regarding this episode. We will look at the state of the science and research of Psilocybin in this three-part series. This episode will go over the mechanism of action, common experience on psilocybin, history, and early research.
There is a burgeoning area of research within psychiatry exploring the use of psilocybin-assisted psychotherapy to treat various conditions. Psilocybin has been part of the larger human experience for millennia. It has been increasingly part of western consciousness for the last 80 years, with popular culture and federal legislation each playing distinct roles in psilocybin’s place in our society today. As the scientific community explores its therapeutic use and safety in controlled settings, there are a lot of people outside of that community who are passionate advocates for its recreational use. Mental health providers are being asked about this form of therapy from their patients. If we are to be knowledgeable about this subject, it is useful to know the sources that our patients are getting their information from, the history of its use, and what we currently know about its safety. We explore these factors in the first episode of this three part series on psilocybin psychotherapy.
Introduction
To discuss the parameters of what we are talking about when we discuss psychedelics we looked at this paper defining the term (Nichols, 2004). People often use the terms to refer to pharmacologically active substances that alter consciousness, can include cannabinoids, MDMA, ketamine, and classic psychedelics like psilocybin, LSD, DMT, and mescaline.
Here, we are referring only to “classic psychedelics” which are serotonergic 5HT2a receptor agonist agents that are chemically similar to psilocybin
Other terms we will use are:
Psychedelics - “mind or soul manifesting”
Entheogen - “the divine within”
The mechanism of action of psilocybin is related to the stimulation or agonism at the 5-HT2A receptor, which is a specific serotonin receptor. The effects of stimulating this receptor is the topic of this series. Medications already exist (specifically antipsychotics) that block or antagonize this receptor which is described in The Stahl’s essential psychopharmacology. (Stahl, 2013)
Blocking this receptor theoretically increases the amount of dopamine in the striatum and tuberoinfundibular pathway, decreasing the risk of extrapyramidal symptoms and hyperprolactinemia typical of first generation antipsychotics.
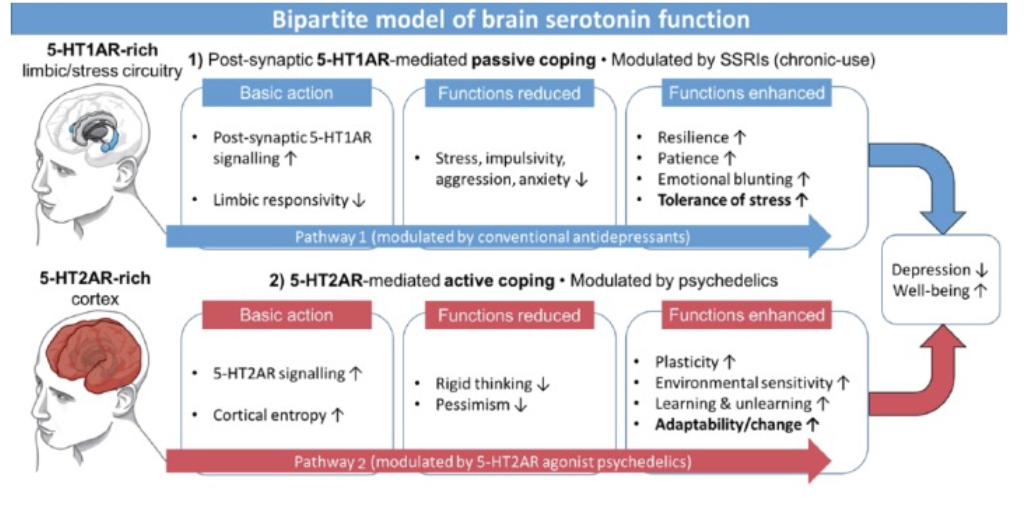
To compare two different serotonin receptors in the brain we looked at a paper called Serotonin and brain function: a tale of two receptors (Carhart-Harris and Nutt, 2017), which proposes two different mechanisms of serotonin in the brain.
This paper proposes that passive coping (i.e. tolerating a source of stress) is the default response to adversity, mediated by postsynaptic 5-HT1A receptor signalling and is characterised by stress moderation. This is reflected by the fact that these receptors are primarily located within “stress circuitry”(midbrain, limbic and cortical regions), and is usually inhibitory in nature. These centers are primarily stimulated by SSRIs.
In contrast, active coping, (i.e. actively addressing a source of stress) is activated when the default response is overwhelmed and is mediated by 5-HT2A signalling and characterised by increasing the capacity for change. This is reflected by the location of these receptors in the cortex and the default mode network, and is usually excitatory in nature. These are the centers that are stimulated by the classic psychedelics.
History of Psilocybin
Natural psychedelic substances (e.g. psilocybin, ayahuasca, peyote) have played a significant role in the development of philosophy and religion in many cultures. Many individuals have argued compellingly that it is the catalyst for many for human’s earliest cultures, philosophies, theologies, and creative developments.
There are prehistoric artifacts that indicate human psilocybin use...
Murals dated 9000 to 7000 BCE found in the Sahara desert in southeast Algeria depict horned beings dressed as dancers, clothed in garb decorated with geometrical designs, and holding mushroom-like objects. Parallel lines extend from the mushroom shapes to the center of the dancers' heads.
6,000-year-old pictographs discovered near the Spanish town of Villar del Humo illustrate several mushrooms that have been tentatively identified as Psilocybe hispanica, a hallucinogenic species native to the area.
More recently, there is evidence of psychedelic use in ancient civilizations
There was a religious rite in Greece for over 200 years known as the Elucinian mysteries. This was secret, all-night ceremony each September that involved a fast followed by drinking a special potion known as “Kykeon”, κυκεών (Ky-key-in).
We know very little about this ceremony, but many suspect that κυκεών was a hallucinogenic brew. The ritual was partially described in the 2nd century A.D.: ‘‘. . .of all the divine things that exist among men, it is both the most awesome and the most luminous.’’
In ancient India they had a food or drink called Soma that is described in Vedic hymns that opened the doors to divine experience and refer to experiences of immortality and light that are characteristic of an psychedelic experience.
“Good fruit containing food not any intoxicating drink, we drink you
You are elixir of life, achieve physical strength or light of god,
achieve control over senses;
In this situation, what our enemy can do to me?
God, what even violent people can do to me?”
Candidate mushrooms for the Soma are suggested by anthropologist Gordon Wasson in the book The Soma of the Rig Veda, n.d.) Most famously, psychedelics mushrooms, also known as Teonanacatl or ‘‘god’s flesh’’ were used by the Aztec shamans as a sacrament and in religious ceremonies. The religious leaders would ingest the entheogens to engage in prophecy, interpret visions, and healing and continue in indigious populations today in sacred ritual.
These ceremonies were forced underground by the Spanish, but were first recorded by Spanish Franciscan friar Bernardino de Sahagún who journeyed to Mexico (“New Spain”) in 1529. This practice was rediscovered by the intellectual western world by an amateur anthropologist and mycologist Gordon Wasson and his wife, Valentina Pavlovna Wasson, who traveled to Oaxaca in Southern Mexico in 1955 and wrote an article in Time magazine that brought awareness of psychedelic mushrooms to the Western world. (Nichols, 2020)
Why, as experts, we should know more about this than the general public… and we may not.
Popular culture constantly talks about the use of psychedelics. One of the most outspoken proponents is the popular podcast host Joe Rogan. He has discussed psychedelics with many guests and his show is an introduction and education for many people on psychedelics.
Some of his guests are:
Dennis McKenna, Rick Doblin, Michael Pollan, Dr. Andrew Weil
His podcast includes the powerful personal experiences of Mike Tyson (5-MeO-DMT) and Paul Stamets (psilocybin)
Other popular outlets with information include the New Yorker, Netflix show Goop lab, 60 minutes episode, and Michael Pollan’s book How to Change Your Mind where he explores the recent history of psychedelic drugs, from the 1960s to the resulting backlash. He discusses the recent resurgence in this field of research, as well as his own personal use of psychedelics.
People sometimes give psilocybin credit for significant parts of human development, such as “Stoned ape theory.” It was first proposed by Terrence McKenna in his book, Food for the Gods, and has been reintroduced by Paul Stamets. It essentially describes that humans that were hunting and tracking animals on the savannah would have access to psychedelic mushrooms in animal dung. These psychedelic experiences would have increased visual acuity, creativity, sexual activity, and help in developing language, expanding consciousness, art, and representational communication as well as allow for the extinction of a maladaptive fear response.
What is the psychedelic experience like?
Wikipedia describes the experience: “Psilocybin can strongly influence the subjective experience of the passage of time. Users often feel as if time is slowed down, resulting in the perception that "minutes appear to be hours" or "time is standing still." Users having a pleasant experience can feel a sense of connection to others, nature, and the universe; other perceptions and emotions are also often intensified. Users having an unpleasant experience (a "bad trip") describe a reaction accompanied by fear, other unpleasant feelings, and occasionally by dangerous behavior. In general, the phrase "bad trip" is used to describe a reaction that is characterized primarily by fear or other unpleasant emotions, not just transitory experience of such feelings. A variety of factors may contribute to a psilocybin user experiencing a bad trip, including "tripping" during an emotional or physical low or in a non-supportive environment (see: set and setting). Ingesting psilocybin in combination with other drugs, including alcohol, can also increase the likelihood of a bad trip.
We also looked at the article What is the psychedelic experience like? (Malone et al., 2018) 10.3389/fphar.2018.00256 where they describe that people experience events with “profound personal meaning” that include re-experiencing “previous traumas”, “their own near-death or death experiences”, “a deep connection with themselves, other people and work around them.”
If you’re re-experiencing traumas and you feel emotionally safe as well as a connection with others, it’s going to change the nature of trauma. That’s often what is done in psychotherapy. When people feel a decrease in shame through a strong therapeutic alliance, empathy, connection, it actually changes the way people experience the trauma.
Safety and adverse effects
We looked at a few published articles to understand the risks and benefits associated with psilocybin use in the general population. To start, we looked at two population studies:
Classic psychedelic use is associated with reduced psychological distress and suicidality in the United States adult population. (Hendricks et al., 2015)
This was a survey with 191,832 individuals that showed that the use of psychedelic drugs such as psilocybin is associated with significantly reduced odds of past month psychological distress, past year suicidal thinking, past year suicidal planning, and past year suicide attempt.
Of note, 98% of people who used psychedelics also used marijuana and/or other drugs. The group in general prior to controlling for the other drug use had worse mental health. This study is controlling for all of the different drug use when it makes statements about if psychedelics are associated with positive mental health. But, we have to ask how did they control for that? It really comes down to the 2% who may only be using psychedelic which is difficult to know if it’s even 2% only using psychedelics because although they may not be using marijuana, but they could be using other drugs such as cocaine. There could be some problems in the study due to this.
Another thought is that correlation doesn’t equal causation. We don’t know if the model specificity is able to map the data in the most accurate way. There are ways that you can use many different models to map the same data and then look at how the models compare to each other which was not done in this study either.
Psychedelics and Mental Health: A Population Study (Krebs & Johansen, 2013)
A survey with 130,152 adults in the United States shows that there is no relationship between lifetime use of psychedelics and any undesirable past year mental health outcomes, including serious psychological distress, mental health treatment (inpatient, outpatient, medication, felt a need but did not receive), or symptoms of panic disorder, major depressive episode, mania, social phobia, generalized anxiety disorder, agoraphobia, posttraumatic stress disorder, or non-affective psychosis.
These studies do their best to isolate psilocybin use, however, it is notable that they control for age, sex, education, income, risky behavior, and every other drug. However, users of psychedelics tend to be whiter, male, richer, more educated, exhibit more risky behavior, and use more illicit substances. There are correlations, but it is unknown if there is also a causative effect.
This study has the same issue as the prior study. The respondents who use psychedelics have increased risky behavior and increased use of every other drug compared to the control group. Did they properly control all the other aspects properly in order to create the most accurate data?
There is a specific DSM diagnosis related to psychedelic use called hallucinogen persisting perception disorder. The DSM criteria consist of:
Following the cessation of use of a hallucinogen, the re-experiencing of one or more of the perceptual symptoms that were experienced while intoxicated with the hallucinogen (e.g., geometric hallucinations, false perceptions of movement in the peripheral visual fields, flashes of color, intensified colors, trails of images of moving objects, positive afterimages, halos around objects, macropsia and micropsia);
The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning;
The symptoms are not attributable to another medical condition (e.g., anatomical lesions and infections of the brain, visual epilepsies) and are not better explained by another mental disorder (e.g., delirium, major neurocognitive disorder, schizophrenia) or hypnopompic hallucinations.
We look at a few studies to understand the prevalence and risks of HPPD and other psychological disorders that result from psilocybin and other psychedelic use.
In the first paper we looked at hallucinogen persisting perception disorder: A literature review and three case reports.(Skryabin et al., 2018) 10.1080/10550887.2019.1673655 essentially discussed that case reports of HPPD have appeared in the literature but are rare.
On a further dive the paper abnormal visual experiences in individuals with histories of hallucinogen use: A web-based questionnaire (Baggott et al., 2011) conducted an online survey with 2,679 participants that indicated that while drug-free visual experiences are common (50% of users) after the use of psychedelics, it is less common, but not rare (4.7% of experiences) for users to have disturbing experiences or seek mental health care after a psychedelic experience. This is evidence that the drugs are not risk-free as they can lead to experiences that are markedly psychologically challenging, particularly in the absence of proper preparation, support, and integration.
I’ve had a patient come to me after they had a really bad trip at a party. He took a drop in his eye and everyone was laughing because it contained LSD. He described this distressing event where he felt completely outside of his body. This is a horrible environment to have a trip because he didn’t want to have one and everyone was laughing at him as though he was the joke of the party. Due to this event he wouldn’t drink out of a drinking fountain or trust public spaces. Psychotherapy sessions re-processing the trauma helped him overcome and return to normal.
To look at the long term positive and negative consequences of psilocybin use, in particular, we read this Survey study of challenging experiences after ingesting psilocybin mushrooms: Acute and enduring positive and negative consequences (Carbonaro et al., 2016) which was an online survey of 1,993 individuals (mean age 30 yrs; 78% male; median of 6-10 prior experiences).
Only 2.1% of responders reported taking psilocybin under conditions similar to the research settings.
The vast majority reported positive outcomes with 84% endorsing benefits from the experience. 39% rated it among the top five most challenging experiences of their lifetime which could be positive or negative depending on the setting and support available.
Six respondents reported that they had pre-existing suicidal thoughts which fully remitted after their psilocybin experience.
Of note there were significant and prevalent negative outcomes reported with 11% reporting they put themselves or others at risk of physical harm, 2.6% behaved in a physically aggressive or violent manner, 2.7% received medical help during the trip, and 7.6% sought treatment for enduring psychological symptoms that continued >1 year after the trip.
Of these there were 3 reported cases of psychosis within a typically vulnerable population, white males between the ages of 18-21.
There were three cases of attempted suicide. Two of them had previously diagnosed with depression and suicide attempts.
3 attempted cases of suicide are intense. In comparison, regarding SSRIs, we know the risk of suicidal thoughts slightly increases in those under 25 years old, but there aren’t any cases in the studies of 10,000+ SSRI use where people actually tried to commit suicide.
This study compared the survey data to the data collected from laboratory settings, where people are screened, prepared, and supported where there have been no reported severe adverse effects.
As of May 2016, Johns Hopkins had 250 volunteers in more than 380 sessions. Of these participants, 3 people had contacted researchers for negative outcomes. One ended up having hyperthyroidism, one had an anxiety attack which was screened by the ED, and one deferred help from a psychologist and sought help from a spiritual counselor, and symptoms resolved within 5 months.
There was another lab that collected adverse events in their participants in the paper Acute, subacute and long-term subjective effects of psilocybin in healthy humans: a pooled analysis of experimental studies.(Studerus et al., 2011)
They had 110 healthy individuals who received a total of 227 doses of psilocybin (ranging from low to high doses). Of those two subjects dropped out of the studies after reporting experiences of strong anxiety, fear of loss of ego control, emerging negative memories, and thoughts during acute drug effects.
Seven participants endorsed negative changes in psychological well-being
Six noted mild changes in concentration, memory, reactivation of problems, or becoming more pensive or introverted that they did not want to seek help for
One participant, a previously stable medical student contacted the researchers after a high-dose session due to emotional instability, anxiety, and depressive feelings, which he attributed to suppressed memories, thoughts, and feelings that he had been confronted with during the psilocybin session. He was set up with a psychotherapist and his symptoms resolved completely within “a few sessions”.
Hippocrates talked about side effects of treatment. It’s a tradition in medicine to look at outcomes and say that they’re not always good. If you get more into the cultish belief of things, they never report bad cases or side effects. That’s why this is a great discussion—we are trying to point out that there are risks and there are some people who couldn’t tolerate doses of psilocybin or long-term effects which could be concerning for some people when determining whether they want to engage in this type of treatment.
With these risks and outcomes in mind, the Johns Hopkins group created guidelines for safety and recommendations in their study Human hallucinogen research: guidelines for safety. (MW Johnson, WA Richards, RR Griffiths, 2008, n.d.)
They warn that it is important not to underestimate the potential risks of hallucinogen exposure, which include:
Panic or fear reactions resulting in dangerous behavior during the time of drug action;
Precipitation or exacerbation of enduring psychiatric conditions;
Long-lasting perceptual disturbances
Development of a pattern of putting self or others at risk when on hallucinogens. They note that there is minimal risk that exposing humans will lead to physical or psychological dependence. While almost all addictive substances have interactions with dopamine this is minimal with psychedelics
Another concern is whether or not it increases the risk of using other substances that are more dangerous since the prior studies we discussed mentioned those who use hallucinogens are more likely to use cocaine or opiates. It’s probably not the first drug they’ve used, but we’re talking about using them in professional settings which could have unknown side effects. (49:00-50:00).
To understand the toxicity and dependence potential of psilocybin we looked at a few articles: Comparison of acute lethal toxicity of commonly abused psychoactive substances (Gable, 2004), (Gable, 2012) (RS Gable, 2006)
They created this graph comparing different substances.
To measure the safety they compare the Effective dose (ED50) to the lethal dose (LD50)
To measure dependence the authors estimate the relative balance between:
How many people who try a drug will continue to use it despite their desire/intention not to
Do people experience withdrawal symptoms when the drug is not available.
Determine how strongly people want to repeat the drug experience as a result of euphoria, confidence, sensuality, novelty, and so forth.
Of note, there are no documented reports of deaths from an overdose of psilocybin or LSD
However, there is an anecdote that there was an Indian elephant who died at the Oklahoma Zoo in 1962 after it was injected with 297 mg of LSD (about three thousand times the human effective dose).
People suspect that the drugs used to try and revive the elephant, ending up killing it, instead of the LSD itself.
Lessons to be learned from MDMA trials
While the previous data showed that the risks with psilocybin in ongoing trials, with proper screening and therapy, are significantly decreased, we wanted to look at the inherent risks of using mind-altering substances in the therapeutic space.
To look at issues that have come up in therapy, we used information from the Multidisciplinary Association for Psychedelic Sciences (MAPS) and an issue that came up in a trial with MDMA that they sponsored. This information was publicized through their own website and Quartz article.
In the incident, one of the therapeutic guides had about a year-long sexual relationship with a participant he had facilitated with his wife.
The sexual relationship started after completing treatment but before completing the trial follow-up. She moved to where the therapists’ lived and continued to have therapy treatments outside of the trial.
In response, MAPS has developed a code of ethics, and more specialized training for their therapists, as well as requiring 2 therapists, preferably of different genders to be co-facilitators.
MDMA is known to elicit feelings of sexual arousal and emotional intimacy, which does not occur with psilocybin so the same concerns with psilocybin do not apply. However, therapy, in general, is an intentionally unequal relationship, and legal standards state that a patient cannot meaningfully consent to a sexual relationship with their psychologist because of the inherent and therapeutically.
While information is not readily available, there are a few studies looking at the issue of sex between therapists and clients. Sex Between Therapists and Clients (Sex Between Therapists and Clients, n.d.). A study published in 2001 described that 4.4% of therapists (7% of male therapists; 1.5% of female therapists) had inappropriate sexual contact with their patients.
Sexual transference exists. When you get close to someone, including a therapist, there is a bond that is created. Especially if the patient has been sexualized early on in their lives. (Sexualized meaning they got an attachment connection to other human beings through sex which makes it a lot more dangerous for them in any relationship where they are getting close to someone.) Is the relationship going to have healthy boundaries or will it be meeting the gratification of the person giving the therapy, which is where the boundaries break-down.
The drug actually elicits feelings of very close emotional intimacy. Those who have taken them said it was something beyond anything they had ever experienced with regards to intimacy with the people they take it with. The connection that people get from MDMA is something that can be found in a similar way to a good therapeutic alliance where the person has incredible amounts of reduced shame. I have had this told to me by a patient who shared his experience both of MDMA but also of our connection from prolonged therapy. Since therapeutic alliance can be a potent connecting point, boundaries are absolutely necessary in order to continue to have meaningful work as a therapist. The cost of a sexual relationship with a client can be high, including losing one’s practice and long-term damage to the patient.
Harm reduction
We do not recommend using psilocybin or other psychedelics, either extra-legally or without appropriate supervision or preparation. Because people are likely to use it regardless of legal status, here is some information about these substances. If you are going to be using LSD or MDMA off the street you should always test them to ensure their safety with test kits
Harm reduction with Psilocybin
There are over 180 different mushrooms that have been discovered that produce psilocybin, all at different potencies. Recreational doses range from 0.1-5 grams of dry mushrooms depending on the species and individual strength of the specimens.
It is rarely available in pure chemical form, which is used in studies and created in labs.
Information from Erowid.org, a non-profit educational & harm-reduction resource about psychoactive drugs, plants, chemicals, indicates that the cost is usually $20-40 per dose. $100-250 per ounce
While there is underground therapy, it can be difficult to find. People anecdotally on Reddit (here and here) indicate that it can cost $450-750 without preparation or post-integration sessions.
Contamination of mushrooms with other substances is extremely rare but has been documented. Safety should always be a concern when ingesting substances from an unknown source.
Harm reduction with LSD
Information was gathered from Erowid
There are most concerns about contamination with LSD. LSD can come in different forms, including blotters (as opposed to pills or liquid), which is a paper form that can only carry maximum of 200 mcg of substance. While limited there are drugs of abuse that can mimic LSD at that dose. Particularly NBOME. NBOME can trigger a less complex introspection than LSD but can produce strong visual and sensory effects. It can cause dangerous physiological side effects. Of note, genuine LSD blotter is tasteless, while most people describe an intense bitterness with 25I-NBOME or 25C blotter.
Early Research in the 1950s-1960s
Albert Hoffman discovered LSD in 1938 working as a researcher for Sandoz Pharmaceuticals in Switzerland. This set of the first periods of research in the 1950’s-1970s, where there was a lot of research with hallucinogens particularly LSD. During this time, there were over 1,000 scientific papers published, 6 international conferences, and it was prescribed as treatment to over 40,000 patients to treat alcoholism, “narcotic use”, recidivism, adjunct to psychotherapy, creativity, sleep, behavior in autism, and schizophrenia. (DEA - Publications - LSD in the US - The Drug, n.d.).
The research came to end with The Controlled Substances Act of 1970. This law created a classification system that was supposed to be made on standardized criteria including potential for abuse, currently accepted medical use in treatment in the United States, and international treaties.
Despite significant evidence to the contrary, it made cannabis, LSD, and psilocybin schedule 1 substances. To put this into perspective it is valuable to get an idea of the different schedules and examples of different substances in each category. The five scheduled drug classifications are:
Schedule 1 substance: Indicating a high abuse potential, no medical use, and severe safety concerns.
Examples include heroin, lysergic acid diethylamide (LSD), marijuana (cannabis), 3,4-methylenedioxymethamphetamine (ecstasy), psilocybin, and peyote
Schedule 2: Drugs with medical use that have a high potential for abuse, with use potentially leading to severe psychological or physical dependence.
Examples include hydrocodone, cocaine, methamphetamine, methadone, hydromorphone (Dilaudid), oxycodone (OxyContin), fentanyl, Adderall, and Ritalin
Schedule 3: moderate to low potential for physical and psychological dependence.
Examples include Tylenol with codeine, ketamine, anabolic steroids, testosterone
Schedule 4: Low potential for abuse and low risk of dependence
Examples include Benzodiazepines, Z-drugs (Ambien), Tramadol
Schedule 5: lower potential for abuse than Schedule IV
Examples include Robitussin, pregabalin,
It is speculated that schedule 1 substances were chosen, because they threatened the moral fabric of the country. This law was written at a time during the Vietnam war and during social upheaval when political entities felt threatened by the social and cultural changes of the 1960’s.
A concern with certain substances is that it can call into question everything you thought to be true. This can open an individual up to brainwashing. Psychological defenses that keep people from being open also keep people from accepting harmful or destructive ideologies.
“Modern Era” Clinical Trials Late 1990s-Present
The structure of the psilocybin-assisted therapy done in clinical trials is variable but has common characteristics. There are often two therapists throughout, one male and one female throughout. There are one or two multi-hour preparation therapy sessions to create the set and setting for the treatment and prepare people for a profound experience. They often review the patient’s life story as well as exploring questions such as:
“What are the most meaningful experiences of your life?”
“Who have been/are the most impactful people in your life?”
“Who have been the most important people in your life?”
“What is the role of religion or spirituality in your life?”
“What have been the most important successes and failures in your life?”
During the psilocybin session itself, therapists encourage introspection, usually recommending people lie down with eyeshades on a couch with a predetermined music playlist. This is followed by 2-4 integration sessions to help consolidate the experiences that people have had and concretize the insights they gain from the experience.
In the next episode, we explore the various clinical trials using psilocybin-assisted psychotherapy that have been conducted.
Conclusion
In this first part we have outlined some of the history of psilocybin, its mechanism of action, how it is represented in popular culture, and what we currently know about its safety. This provides a background to some of the further discussions that we will have in the next two parts of this series, where we discuss the different clinical trials that have been conducted, how it affects people and their personalities and the future of this research.
Resources:
Drug Toxicity. (2012, February 20). Robert Gable. https://rgable.wordpress.com/drug-toxicity/